Alternatives to GLP-1: What Works When GLP-1 Drugs Don’t Fit
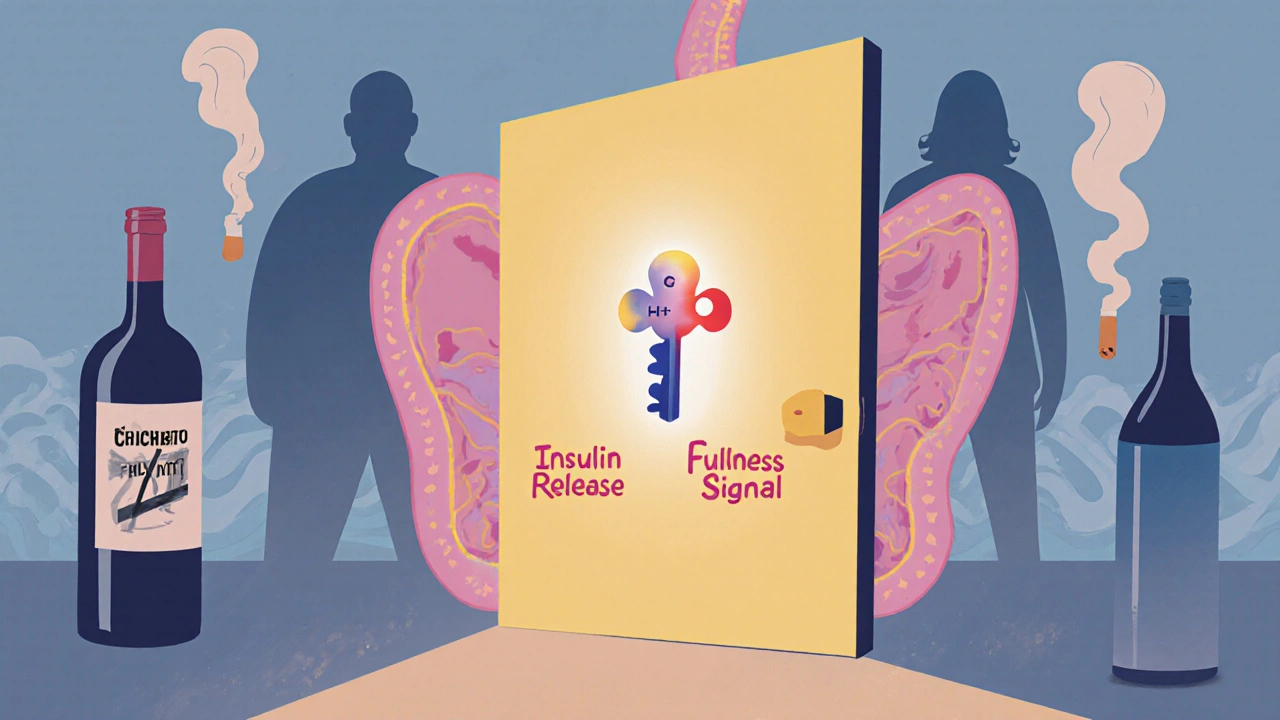
When people talk about GLP-1, a class of drugs that mimic a hormone to control blood sugar and reduce appetite. Also known as glucagon-like peptide-1 receptor agonists, it includes popular medications like semaglutide and liraglutide—used for type 2 diabetes and weight loss. But not everyone can take them. Side effects, cost, or medical history might make GLP-1 drugs a poor fit. That’s where insulin sensitizers, medications that help your body use insulin more effectively come in. Drugs like metformin have been the backbone of type 2 diabetes care for decades. They don’t cause weight gain, are cheap, and work well for people with insulin resistance. Many patients who can’t tolerate GLP-1 drugs find stable control with metformin alone—or paired with other agents.
Then there’s appetite suppressants, drugs that target brain signals to reduce hunger. Unlike GLP-1 drugs that slow digestion and reduce cravings over time, these act faster. Phentermine, for example, is still used in short-term weight management, especially when combined with topiramate (Qsymia). It’s not for everyone—especially those with heart conditions—but for some, it’s a practical stopgap or long-term option when GLP-1s aren’t available. Even newer options like naltrexone-bupropion (Contrave) work differently, targeting both reward pathways and appetite centers in the brain.
For those managing both diabetes and weight, SGLT2 inhibitors, a class of drugs that make your kidneys flush out extra sugar offer a compelling alternative. Drugs like empagliflozin and dapagliflozin don’t just lower blood sugar—they also help with weight loss, lower blood pressure, and protect the heart and kidneys. Studies show they can reduce hospitalizations for heart failure, something GLP-1 drugs don’t always do as clearly. And unlike GLP-1s, they’re often taken as pills, not injections.
Some people turn to older diabetes drugs like sulfonylureas or thiazolidinediones, but those come with trade-offs: weight gain, low blood sugar, or fluid retention. They’re not first choices anymore, but in specific cases—like older adults with limited access to newer meds—they still have a role. Meanwhile, lifestyle changes remain powerful. Research consistently shows that even modest weight loss (5–10% of body weight) through diet and movement can reverse prediabetes and improve insulin sensitivity more reliably than many pills.
You don’t need to chase the latest GLP-1 hype to get results. The real question isn’t whether GLP-1 drugs are better—it’s whether they’re right for you. Some people lose weight and feel great on them. Others find relief, stability, and even better outcomes with other tools. The key is matching the treatment to your body, your health goals, and your daily life—not just the trend.
Below, you’ll find real comparisons of medications, side effect breakdowns, and practical advice from people who’ve tried multiple options. Whether you’re looking for a pill instead of a shot, a cheaper option, or a different way to manage your weight and blood sugar, the posts here give you the facts—not the marketing.
GLP-1 Agonists and Pancreatitis Risk: What You Need to Know About Monitoring and Alternatives
GLP-1 agonists like Ozempic and Wegovy offer major health benefits but carry a debated pancreatitis risk. Learn who's truly at risk, how to monitor for symptoms, and safer alternatives based on the latest 2025 research.
More