Minocin: What You Need to Know
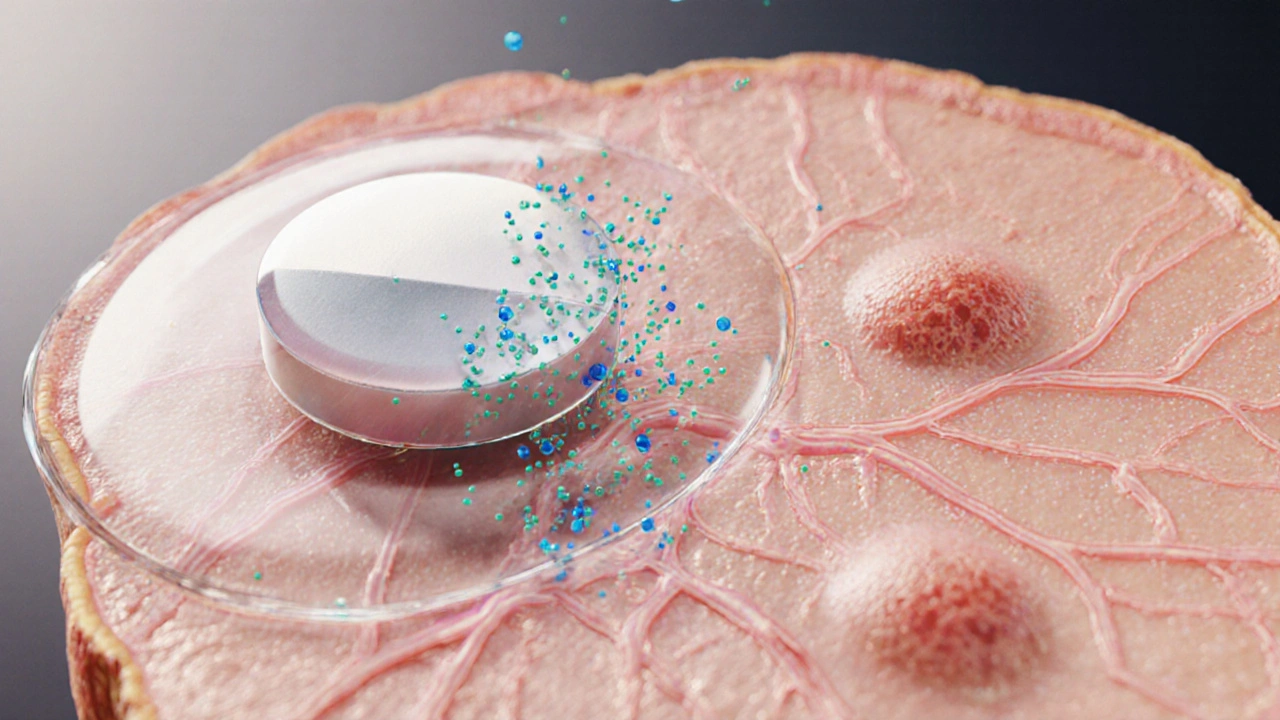
When working with Minocin, a brand of the tetracycline antibiotic minocycline. Also known as minocycline, it’s used to fight bacterial infections and clear stubborn skin problems such as acne. It belongs to the tetracycline class of antibiotic agents that stop bacteria from making proteins, which stalls their growth and eventually kills them. This simple mechanism makes Minocin a go‑to choice for dentists, dermatologists, and primary‑care doctors alike.
How Minocin Works and When It’s Used
Because Minocin targets a broad range of bacteria, doctors prescribe it for everything from moderate acne to respiratory infections, urinary tract infections, and certain sexually transmitted infections. The drug’s ability to get into skin cells helps clear deep‑seated lesions that other topical treatments can’t reach. When a patient starts a course, the usual adult dose is 100 mg twice daily, but doctors may adjust the schedule based on the infection type, kidney function, and patient weight. For teenagers battling severe acne, a typical regimen is 50 mg once a day after a short loading phase, which helps reduce the risk of stomach upset.
Side effects are generally mild but worth watching. The most common complaints are nausea, dizziness, and photosensitivity – meaning you should wear sunscreen and avoid prolonged sun exposure while on Minocin. A rarer but serious risk is drug‑induced lupus, which shows up as joint pain, fever, and a distinctive rash. If any of these symptoms appear, stop the medication and contact a healthcare professional right away. Because Minocin can affect liver enzymes, patients taking other prescription drugs should discuss potential interactions, especially with blood thinners or seizure medications.
Resistance is another factor that shapes how clinicians use Minocin. Overuse or incomplete courses can allow bacteria to develop mechanisms that bypass the drug’s action, making future infections harder to treat. That’s why it’s crucial to finish the full prescribed course, even if symptoms improve early. For pregnant or nursing women, Minocin is generally avoided unless the benefits clearly outweigh the risks, as it can cross the placenta and appear in breast milk.
Having a clear picture of what Minocin does, when it’s appropriate, and how to use it safely empowers you to make informed decisions about your health. Below you’ll find a curated list of articles that dive deeper into specific scenarios—whether you’re looking for dosage calculators, side‑effect management tips, or comparisons with other antibiotics. Explore the collection to find practical advice that matches your situation.
Minocin (Minocycline) vs. Common Antibiotic Alternatives - Full Comparison
A practical guide comparing Minocin (minocycline) with key antibiotic alternatives, covering uses, side effects, cost, and how to choose the right option.
More