Why Alpha-Blockers Are Suddenly a Hot Topic in UTI Management
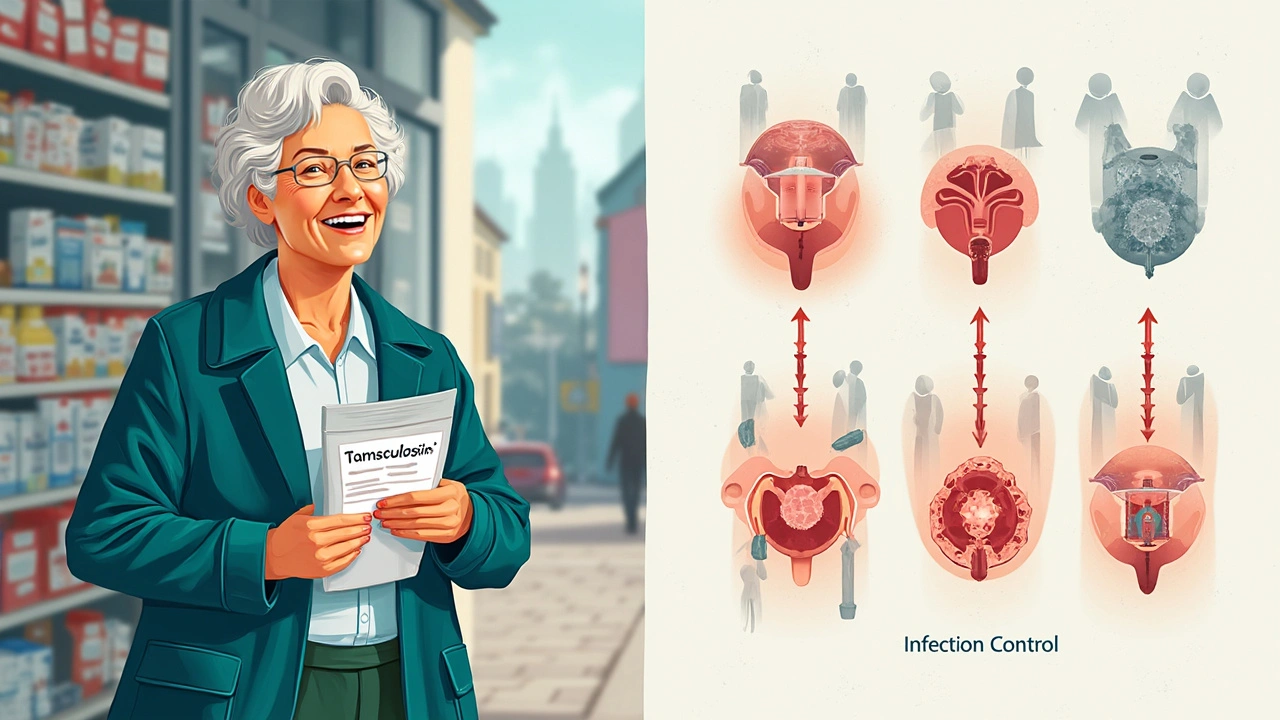
If you’d told most urologists ten years ago that alpha-blockers like tamsulosin would become a frontline topic in infection management, they might have looked at you like you’d tried to bring your Golden Retriever into the operating theater. Tamsulosin, as many know, was designed as an answer to benign prostatic hyperplasia (that fun “can’t pee, can’t sleep” routine for older men). Doctors prescribed it so men could sleep through the night without running to the bathroom every fifteen minutes. So why are we talking about using it for complicated urinary tract infections (UTIs), especially in 2025?
Here’s the twist—alpha-blockers don’t just relax muscles in the prostate. They work all along the lower urinary tract: bladder, sphincters, urethra. When a UTI hits and swelling or infection clogs the flow, tamsulosin’s smooth muscle relaxation can help clear that roadblock. There’s data now suggesting that in men—and sometimes women—who develop serious, so-called “complicated” UTIs (the ones that love to linger, come with fever, or refuse to leave even after rounds of antibiotics), combining standard meds with alpha-blockers can help out. Some recent studies have shown that patients on tamsulosin alongside antibiotics often report fewer return infections and fewer emergency visits for painful retention or severe symptoms.
Maybe you’ve never heard of a UTI turning into a massive problem. If you have, you know these things can spiral. Infections that spread, turn septic, or get stuck behind a swollen prostate or a swollen bladder are not only miserable but can be genuinely dangerous. Now, with the world’s population aging, more people—men and women—are experiencing the combo of a sluggish urinary system and tricky infections. Doctors and patients want to avoid hospital stays and catheters whenever possible (trust me, those are nobody’s idea of a fun weekend). That’s why a medication like tamsulosin—one that’s already sitting in a lot of bathroom cabinets—has people in urology excited all over again.
So, what happens when someone with a complicated UTI adds tamsulosin to their regimen? The immediate effect is that urine tends to pass more freely, even if inflammation is slowing things down. This seemingly small change lowers the catheter risk and gives antibiotics a boost, flushing out bugs rather than trapping them in the bladder. Interestingly, a 2024 multicenter trial from Europe reported that about 35% fewer men needed emergency catheterization for UTI-related retention when taking tamsulosin with their antibiotics versus just antibiotics alone.
What about women? They have less prostate tissue, but don’t tune out. Some clinics have found that women who’ve had bladder outlet obstruction from infection-related swelling are also seeing benefit—especially in cases after surgery, pelvic injury, or recurring infections with narrowing. As a result, 2025 guidelines are being rewritten in some places to allow a trial of tamsulosin before calling in the surgical team.
But the most game-changing application of alpha-blockers isn’t just about symptom relief. There’s emerging buzz around whether speeding up urinary flow could actually make antibiotics more effective. The “washout” effect hasn’t been nailed down in every study, but some infectious disease doctors swear by it. More urine, more flushing, fewer bacteria hanging around to regroup and reinfect. The consensus? If you can avoid a stay in the hospital or a traumatizing self-catheterization lesson, it’s worth considering.
For more on how alpha-blockers like tamsulosin might help with tricky UTIs and a breakdown of studies, see this tamsulosin UTI guide, which pulls together important facts and what to ask your doctor if you’re on the fence.
Here’s the thing nobody talks about: tamsulosin is not a magic bullet. Some patients experience dizziness or drop in blood pressure, especially when they stand up too fast. It’s also not ideal for everyone—kids, pregnant women, and folks taking certain heart meds should steer clear without close doctor supervision. But as a short-term rescue plan for those stuck in the revolving door of UTIs and ER visits, alpha-blockers have entered a new era. Talk to any urologist attending national meetings this year, and alpha-blockers and infection management are suddenly getting prime-time attention.

How Tamsulosin and Similar Drugs Could Change UTI Treatment Protocols in 2025
Pop quiz: what’s the biggest challenge with complicated UTIs? It’s not just the infection—it’s the domino effect when swelling or pain causes someone to hold urine, can’t empty by themselves, or ends up with retention. Suddenly, everything gets riskier. That’s why health systems are reconsidering how alpha-blockers could step between basic treatment and invasive care. In 2025, doctors are writing new playbooks in clinics and hospitals. Let’s break down how.
Step one: Identify who actually needs an alpha-blocker. Not everyone with a UTI does. But for adults who show “significant voiding dysfunction”—meaning, the infection is making it hard to get pee out—a urologist may recommend tamsulosin for a short-term kickstart. If you walk into a clinic struggling to empty your bladder, have an inflamed prostate, or are post-surgery and worried about trapping infection, this is where the conversation starts. Urologists want to reduce catheter use because catheters can introduce new bacteria, which means a set-back or, worse, hospital stay. So, doctors prescribe tamsulosin for a week or two, tracking if symptoms improve and if the patient can void on their own.
An interesting tip: patients on alpha-blockers should drink extra fluids unless another health issue requires fluid restriction. This helps speed along the “washout” effect, flushing bacteria out faster.
You might be asking, “Do most doctors actually use this approach?” According to the American Urological Association’s latest guidance, more than 40% of urologists in larger cities have started offering alpha-blocker add-ons for recurrent complicated UTIs. The trend is picking up steam outside major hospitals too, especially in regions with a lot of retired folks or those with chronic issues that slow down urination. Some urgent care clinics now have standing orders for tamsulosin when a patient comes in with both infection and classic signs of retention.
- Tip for patients: If you’re prescribed tamsulosin for a UTI, keep track of dizziness, lightheadedness, or sudden drops in energy. The first dose can catch people off guard (ask me how I know—remind me to tell you about the time I thought I could walk Max after my own first dose). It’s smart to take the pill at night, right before lying down.
- Tip for caregivers: Watch older loved ones closely when starting tamsulosin. They might stand up and wobble or lose balance in the first few days. It’s worth setting up a call with the doctor to check if symptoms are more than expected.
- Always double check existing medications. Tamsulosin has known interactions—some blood pressure or antifungal meds just don’t mix well. Bring a complete med list to every appointment.
A major change in 2025 is pharmacists working directly with doctors to spot risky combos and help patients transition off alpha-blockers once their UTI is under control. There’s new software alerting prescribers to drug-drug risks—something I wish existed when my own aunt landed in the ER after a prescription mix-up. Smart systems are keeping real people safer.
One more surprising angle: alpha-blockers may also lower pelvic pain that comes with infections. In chronic conditions like interstitial cystitis, some clinics reported up to a 45% reduction in pain flares when patients took tamsulosin during infection episodes, though this is still a developing area of research.
All these applications boil down to something simple: making sure more people can stay home, keep their dignity, and avoid repeat hospitalizations. That’s a win for quality of life and the healthcare system. The more you know about your options, the better decisions you (or your family) can make. If your doctor hasn’t mentioned alpha-blockers as part of your infection rescue plan, bring it up—sometimes the best solutions are hiding in plain sight.
Where Research and Real Life Meet: Forecasts, Myths, and Practical Tips
The buzz around alpha-blockers in UTI management is already leading to some wild predictions. Will every stubborn infection eventually get paired with tamsulosin? That’s a stretch, at least for now. Ongoing trials are looking at exactly who benefits most: men with enlarged prostates, women with pelvic narrowing, and elderly patients who struggle with complete bladder emptying. Not every patient needs an alpha-blocker, but the focus is now on using it as a bridge—something to help patients recover faster while avoiding long-term side effects or unnecessary surgery.
Let’s address a persistent myth: tamsulosin is not an antibiotic. It doesn’t kill bacteria. Instead, it works by knocking down the barriers that keep infected urine from leaving the body. Used wisely, it improves the odds of clearing infections when paired with trusted antibiotics. Anyone trying to avoid antibiotics or looking for a natural cure should know: this isn’t a vitamin supplement and should never replace proper microbial treatment.
For those worried about side effects, the good news is most people tolerate short-term alpha-blockers pretty well. Typical side effects include mild dizziness, lightheadedness, and sometimes stuffy nose or reduced ejaculation in men. Long-term use carries more risks, but in infection management, most people are only on the medication for a week or two. Still, if there’s a sudden spike in fatigue or a scary fall, get medical help; better safe than sorry. It’s never embarrassing to ask, especially if you’re taking care of an older parent, like I once did—nurses have seen it all.
Got pets who are nosy? My own Fluffy—a purebred Persian—once batted a tamsulosin capsule off my nightstand. Luckily, Max didn’t eat it, but keep all meds locked away, especially with curious critters around. This stuff is for humans only, and pet ERs are busier than ever with accidental ingestions.
When it comes to monitoring progress, most doctors now recommend a simple tracking sheet—marking down symptoms, urinary output, and any side effects for the first week. It might feel tedious, but a data-driven conversation saves time and confusion at follow-ups. More clinics are offering secure portals for patients to upload symptom logs, which helps adjust doses and catch rare side effects earlier.
| Scenario | Possible Use of Tamsulosin | Expected Benefit | Risk Concerns |
|---|---|---|---|
| Man with UTI, enlarged prostate, urinary retention | Short course (7-14 days) | Lower catheter risk, faster recovery | Blood pressure drop, dizziness |
| Woman post-pelvic surgery, recurrent UTIs | Short-term use under supervision | Improved voiding, faster infection clearance | Lightheadedness, rare allergic reactions |
| Elderly with chronic incomplete emptying + UTI | Careful trial, monitor closely | Avoids hospital, supports at-home recovery | Falls, med interactions |
| Young patient with ‘simple’ UTI, normal bladder | Not recommended | No proven advantage | Unnecessary side effects |
Looking ahead, expect more home monitoring: digital urinals, connected apps, and better patient education about the “gray zone” between antibiotics and surgery. Research is also testing new alpha-blocker formulas that might be safer for women, those on complex med regimens, or people with kidney problems. In Europe and parts of Asia, clinical trials are underway on slow-release versions and combo meds that target multiple bladder symptoms at once.
For patients and caregivers navigating complicated UTIs in 2025, alpha-blockers offer a fresh line of defense—one that doesn’t replace core infection treatment but might prevent a spiral into the ER. As always, open talks with your doctor, careful symptom tracking, and a healthy dose of skepticism about miracle cures will keep you a step ahead. With advancing research and better digital tools, managing these frustrating infections is getting a little less daunting—one tablet, one flush, one log at a time.


Jillian Rooney
It baffles me how some doc's ignore basic common sense and sprinkle foreign guidelines on our patients. We should stick to good ol' American urology standards, not some overseas fad.
Rex Peterson
The integration of pharmacologic smooth‑muscle relaxation into antimicrobial stewardship raises profound questions about the ontology of therapeutic synergy. One must consider whether we are merely augmenting the kinetic milieu of urine flow or reshaping the epistemic framework of infection control. In this regard, tamsulosin serves as a catalyst that blurs the line between adjunctive and primary treatment modalities. Such a paradigm shift compels a reevaluation of clinical heuristics that have long governed urologic practice. Ultimately, the ethical imperative is to balance efficacy with the potential for iatrogenic compromise.
Candace Jones
For patients starting a short course of tamsulosin during a complicated UTI, it’s wise to schedule a fluid intake of at least 2‑3 L per day, divided throughout waking hours. Maintaining a simple symptom diary-recording voiding frequency, any dizziness, and pain levels-helps the clinician fine‑tune therapy. Also, advise taking the dose at bedtime to minimize orthostatic symptoms upon rising.
Robert Ortega
Both the antimicrobial and the alpha‑blocker target different aspects of the infection cascade, and when used judiciously, they can complement each other without necessarily increasing adverse events. It’s a matter of patient selection and monitoring rather than a blanket protocol.
Elizabeth Nisbet
Hey there, if you’re worried about the dizziness, just make sure to stand up slowly and keep a glass of water handy. Most folks feel fine after the first day, and the extra urine flow can really speed up recovery.
Sydney Tammarine
Oh, the drama of a seemingly simple UTI turning into a heroic saga of bladder conquest! 🌟 One must applaud the audacity of clinicians who dare to blend tamsulosin with antibiotics-truly a renaissance of urologic ingenuity. Yet, let us not forget the moral weight of prescribing a potent vasodilator without due caution; the stakes are as lofty as the heavens. 🙏
josue rosa
In addressing the rhetorical flourish presented above, it is incumbent upon the practitioner to delineate the pharmacodynamic interface between α‑adrenergic antagonism and antimicrobial efficacy. The mechanistic premise predicates upon the alleviation of urethral and vesical smooth‑muscle spasm, thereby augmenting the hydro‑dynamic clearance of bacteriuric load. Empirical data from multicenter European cohorts, as referenced in the primary article, corroborate a statistically significant reduction in catheter‑related interventions when tamsulosin is co‑administered. Moreover, the hemodynamic profile of tamsulosin warrants vigilant assessment of orthostatic hypotension, particularly in geriatric cohorts with comorbid autonomic dysregulation. The temporal window of therapeutic benefit appears confined to a 7‑14‑day interval, aligning with the acute phase of bacterial proliferation and host inflammatory response. It is plausible to hypothesize that the enhanced urinary throughput serves as a mechanical adjunct to antibiotic diffusion gradients, thereby optimizing tissue penetration. Nonetheless, the literature remains equivocal regarding the magnitude of this “washout” effect, necessitating further randomized controlled trials with stratified subpopulations. From a health‑economics perspective, the reduction in emergency department visits translates into appreciable cost savings and mitigates the iatrogenic sequelae of indwelling catheters. Clinicians should thus integrate shared decision‑making frameworks, wherein patients are apprised of both the potential amelioration of voiding dysfunction and the attendant risk spectrum. The ethical dimension of prescribing a vasoactive agent for infection control must be weighed against the principle of non‑maleficence. In practice, the confluence of pharmacological synergy and patient‑centered care epitomizes the evolving paradigm of precision urology. Consequently, while the dramatization of therapeutic innovation is intellectually stimulating, it must be anchored in rigorous evidence and prudent clinical judgment. Finally, interdisciplinary collaboration among urologists, infectious disease specialists, and primary care providers will ensure that such adjunctive strategies are deployed judiciously, thereby safeguarding patient outcomes while advancing the frontiers of therapeutic integration. Future investigations may also explore selective α1‑blocker subtypes to minimize systemic effects. Such nuanced pharmacologic tailoring could further refine the risk‑benefit calculus in complex urinary infections.
Shawn Simms
While the preceding contributions are largely informative, there are several orthographic inconsistencies that warrant correction. For instance, “doc’s” should be rendered as “doctors,” and “urology” is misspelled. Precise language is essential in medical discourse to avoid ambiguity. Moreover, the use of “&” in formal writing is discouraged; the conjunction “and” is preferable. Finally, proper citation of the 2024 multicenter trial would strengthen the argument.
Geneva Angeles
Let’s get real-this is exactly the kind of breakthrough we need to kick those stubborn UTIs to the curb! By combining a tried‑and‑true alpha‑blocker with antibiotics, we’re not just treating symptoms; we’re actively flushing out the culprits and shortening recovery times. The data shows a clear drop in emergency catheterizations, which means fewer hospital trips and more quality time at home. It’s a win‑win for patients, providers, and the healthcare system alike. So, if you’ve been battling recurrent infections, demand that your doctor consider this regimen-don’t settle for outdated monotherapy. The future is already here, and it’s flush‑forward!
Scott Shubitz
Wow, you just turned a clinical discussion into a Broadway show, didn’t you? Let’s not dress up a modest adjunct therapy as a miracle cure. The reality is that tamsulosin adds a modest benefit at best, and the hype can mislead patients into over‑relying on a pill that may cause dizzy spells. While I applaud your enthusiasm, let’s keep the flamboyance in check and remember that antibiotics remain the frontline hero.
Michael Wall
We must not abandon proven protocols for trendy shortcuts.
Christopher Xompero
Honestly, anyone who thinks a fancy alpha‑blocker can replace solid antibiotic regimens is living in a fantasy-it's like swapping a scalpel for a butter knife in surgery.
Irene Harty
Given the undisclosed financial incentives from pharmaceutical conglomerates, one might reasonably suspect that the promotion of tamsulosin as an adjunctive agent in urinary tract infections serves interests beyond pure patient welfare; the intricate web of lobbying, research funding, and regulatory capture necessitates a critical appraisal of the underlying data.
Jason Lancer
Another hype piece, same old story: pill, promise, repeat.
Brooks Gregoria
If the prevailing narrative claims that alpha‑blockers are a panacea for complicated UTIs, then we must ask whether this consensus is derived from rigorous evidence or merely from the echo chamber of contemporary urologic fashion.