Anticoagulant Dosing Calculator
Please enter patient information and click "Calculate Dose" to see recommendations.
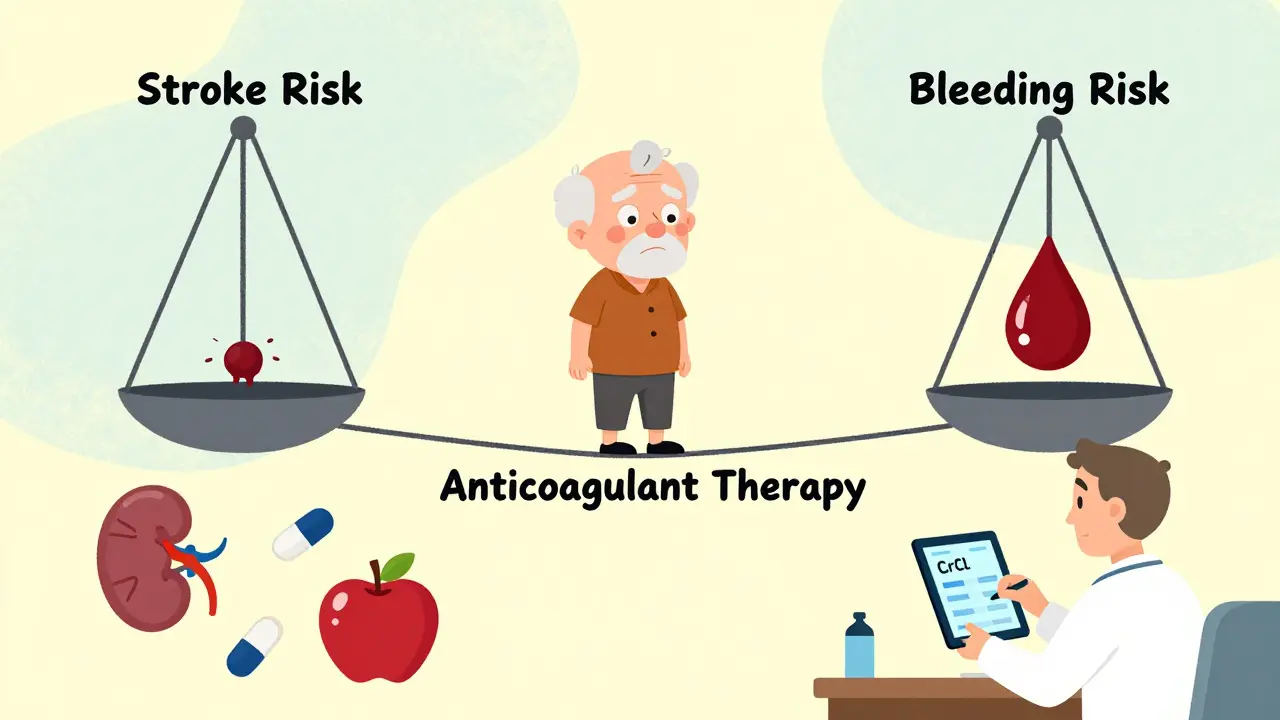
When someone is prescribed a blood thinner, the goal is simple: stop dangerous clots before they form. But every time a patient takes an anticoagulant, they’re walking a tightrope. One slip - a fall, a cut, a missed dose, or a drug interaction - and the risk of uncontrolled bleeding skyrockets. Hemorrhage isn’t just a side effect; it’s the most dangerous complication of anticoagulant therapy, responsible for tens of thousands of hospital visits every year in the U.S. alone.
Why Blood Thinners Are So Dangerous
Anticoagulants don’t actually thin your blood. They interfere with the body’s natural clotting process. That’s useful if you have atrial fibrillation, a mechanical heart valve, or a history of deep vein thrombosis. But it’s risky if you’re 80 years old, have kidney trouble, or take aspirin on the side. The most common anticoagulants fall into three groups: warfarin, heparins, and direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, and dabigatran. Each works differently. Warfarin blocks vitamin K, which your liver needs to make clotting proteins. Heparins boost a natural anticoagulant called antithrombin. DOACs directly block clotting factors - either thrombin or factor Xa. The problem? These drugs have no safety net. Unlike insulin or blood pressure meds, where you can adjust the dose based on how you feel, anticoagulants need precise levels in your blood. Too little, and you get a stroke. Too much, and you bleed out.Who’s at Highest Risk for Bleeding?
Not everyone on blood thinners bleeds. But some people are far more vulnerable. Age is the biggest factor. People over 75 have two to three times the risk of major bleeding compared to younger adults. That’s because kidneys slow down with age, and kidneys are how most DOACs leave the body. If your kidneys aren’t working well, the drug builds up. Renal impairment is another silent killer. If your creatinine clearance (CrCl) drops below 50 mL/min, your bleeding risk doubles. For DOACs like rivaroxaban, that means you need a lower dose. For apixaban, you need to cut the dose if CrCl is below 25 mL/min. Many doctors miss this. A 2023 study found nearly 40% of elderly patients on DOACs were given the wrong dose because kidney function wasn’t checked properly. Other high-risk groups include people with uncontrolled high blood pressure, those on multiple blood-thinning drugs (like aspirin plus warfarin), and anyone with a history of ulcers or brain bleeds. Even something as simple as a fall on the stairs can turn deadly if you’re on a DOAC and your kidneys aren’t checked.Warfarin vs. DOACs: Which Is Safer?
For years, warfarin was the only option. It’s cheap - about $4 a month - but it’s a nightmare to manage. You need regular blood tests (INR) to make sure your level is in the sweet spot: usually between 2.0 and 3.0. If your INR is 4.0 or higher, you’re at serious risk of bleeding. And even then, your diet matters. Eating a lot of leafy greens? That can throw off your INR. DOACs changed everything. They don’t need daily blood tests. They work the same whether you eat broccoli or steak. And they’re safer. Clinical trials show DOACs cause 19-20% fewer major bleeds than warfarin. Apixaban, in particular, has the best safety record - 31% lower bleeding risk than warfarin in the ARISTOTLE trial. But DOACs aren’t perfect. They cost $500-$600 a month without insurance. They don’t have easy reversal agents. And they’re useless in certain cases. If you have a mechanical mitral valve, DOACs can actually increase your risk of stroke. Warfarin is still the gold standard there. Same with antiphospholipid syndrome - DOACs fail more often than warfarin in those patients.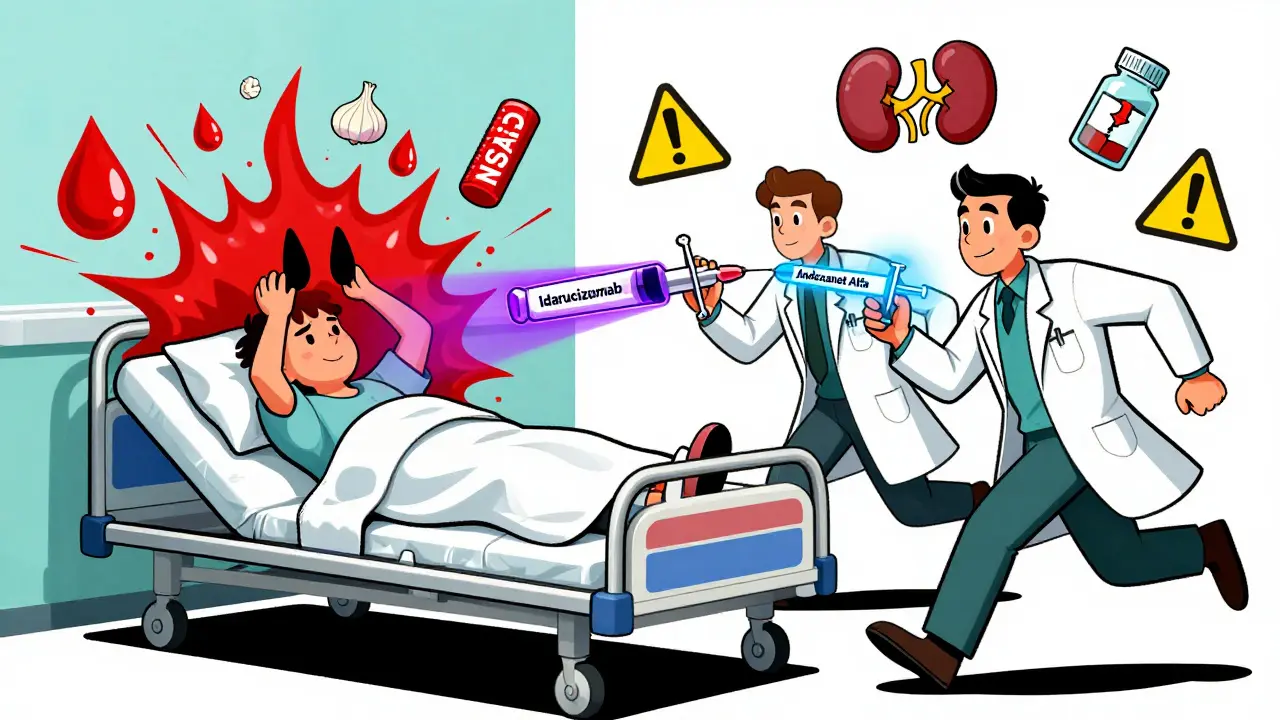
How to Prevent Bleeding Before It Happens
Prevention starts before the first pill is taken. Here’s what works:- Check kidney function first. Always test CrCl before starting any DOAC. Repeat every 3-6 months. If you’re over 75 or have diabetes, test every 3 months.
- Avoid dual antiplatelet therapy. Taking aspirin or clopidogrel with a blood thinner? That increases bleeding risk by 50-70%. Only do it if you absolutely have to - like after a stent.
- Review every medication. Antibiotics, NSAIDs, and even some herbal supplements (like ginkgo or garlic) can boost bleeding risk. A 2022 study found 68% of patients on anticoagulants were taking at least one interacting drug.
- Use the right dose. Apixaban is often overprescribed at 5 mg twice daily in elderly patients. The correct dose for those over 80 or under 60 kg is 2.5 mg twice daily. Many doctors don’t know this.
- Don’t stop cold turkey. Stopping anticoagulants suddenly can cause rebound clots. Always consult your doctor before quitting.
What to Do If Bleeding Starts
If someone on anticoagulants starts bleeding - nosebleed that won’t stop, vomiting blood, sudden severe headache, swelling in the leg - time is critical. Don’t wait. Call 911. But if you’re a clinician or a caregiver, here’s what you need to know:- For warfarin: Give 4f-PCC (four-factor prothrombin complex concentrate) at 25-50 units/kg. It fixes INR in 15 minutes. Vitamin K helps too, but it takes hours. FFP (fresh frozen plasma) is outdated - it takes too long to thaw and isn’t as effective.
- For dabigatran: Use idarucizumab. It’s a specific antidote. One 5g IV dose reverses the drug in minutes.
- For apixaban, rivaroxaban, edoxaban: Use andexanet alfa. It’s expensive - around $13,000 per dose - but it works. It’s the only approved reversal agent for factor Xa inhibitors.
- For heparin: Use protamine sulfate. It neutralizes unfractionated heparin well, but only partially reverses low-molecular-weight heparins like enoxaparin.
Reversal Agents: The New Lifeline
Before 2015, there was no way to quickly reverse DOACs. If a patient bled, doctors had to wait for the drug to wear off - which could take days. That meant many people died from preventable bleeds. The approval of idarucizumab for dabigatran and andexanet alfa for factor Xa inhibitors changed that. These aren’t just drugs - they’re emergency tools. They turn a potentially fatal situation into a manageable one. But access is uneven. Rural hospitals may not stock them. Insurance may deny coverage. And many ER staff still don’t know they exist. A 2023 survey found only 52% of emergency departments had andexanet alfa on hand. That’s unacceptable.
When to Restart Anticoagulation After Bleeding
This is one of the hardest decisions in medicine. Do you restart the blood thinner? Or let the patient live with the risk of stroke? The American College of Cardiology gives clear guidance:- If the bleeding was minor - like a nosebleed or small bruise - restart within 1-3 days.
- If it was major - like a GI bleed or brain hemorrhage - wait 7-14 days, depending on the cause.
- If the patient has a high stroke risk (CHA₂DS₂-VASc score ≥2), restart as soon as possible. The risk of another clot is higher than the risk of re-bleeding.
- If the patient has low stroke risk - say, a provoked DVT that’s been treated for 3 months - you might consider stopping forever.
The Future: Better Tools on the Horizon
Scientists are working on breakthroughs. One is ciraparantag - a universal reversal agent that could undo all anticoagulants with a single shot. It’s in late-stage trials and could be available by 2027. Another is point-of-care testing for DOACs. Right now, you can’t check apixaban levels like you check INR for warfarin. New tests are being developed that could give results in 10 minutes at the bedside. That could reduce bleeding events by 15-20%. And then there’s personalized dosing. Genetic testing may soon tell us who metabolizes DOACs slowly, who needs lower doses, and who’s at risk for bleeding even at standard doses.Final Thought: It’s Not About Avoiding Blood Thinners - It’s About Using Them Right
Anticoagulants save lives. But they kill too - often because we treat them like ordinary pills. They’re not. They’re precision tools. And like any precision tool, they demand respect. The answer isn’t to avoid them. It’s to use them wisely. Check kidneys. Avoid interactions. Know the reversal agents. Restart when safe. And never assume - always verify.Every time you prescribe or take a blood thinner, you’re choosing between two dangers. The trick is to tilt the scale toward safety - not by avoiding the drug, but by mastering it.
Can you reverse DOACs at home?
No. Reversal agents like idarucizumab and andexanet alfa are only available in hospitals and require IV administration. If you suspect bleeding while on a DOAC, call emergency services immediately. Do not wait or try to manage it yourself.
Is warfarin still used today?
Yes. Warfarin is still first-line for mechanical heart valves (especially mitral valves) and antiphospholipid syndrome. DOACs are less effective in these cases and carry higher clotting risks. Warfarin is also used when cost is a major barrier, since it costs less than $5 a month.
How often should kidney function be checked on DOACs?
At least once when starting the drug, then every 3-6 months for stable patients. For those over 75, with kidney disease, or on other nephrotoxic drugs, check every 3 months. Some guidelines recommend checking before each refill if the patient is frail or has fluctuating kidney function.
Can you take NSAIDs like ibuprofen while on blood thinners?
Avoid them if possible. NSAIDs increase the risk of stomach bleeding and can worsen kidney function. Use acetaminophen (Tylenol) instead for pain. If you must use NSAIDs, do so only under close supervision, for the shortest time possible, and with a proton-pump inhibitor like omeprazole to protect your stomach.
Do all DOACs have the same bleeding risk?
No. Apixaban has the lowest bleeding risk among DOACs - about 31% lower than warfarin. Dabigatran has slightly higher GI bleeding risk. Rivaroxaban carries a higher risk in patients with poor kidney function. Edoxaban is similar to apixaban but less studied. Always choose based on individual risk factors, not just cost or convenience.
What should you do if you miss a dose of your blood thinner?
If you miss a dose of a DOAC and remember within 6 hours of your scheduled time, take it right away. If it’s more than 6 hours late, skip it and take your next dose at the regular time. Never double up. For warfarin, contact your provider - they may adjust your next dose based on your INR. Never guess.

laura Drever
lol so many words for something simple: dont take NSAIDs, check kidneys, dont stop cold turkey. why do docs even write essays?
Diana Campos Ortiz
I'm a nurse and this is spot on. I've seen too many elderly patients on rivaroxaban with CrCl under 30 and no one caught it. One lady bled into her abdomen from a fall that looked like a bump. We almost lost her. Always check the labs. Always.
Also, ginkgo biloba? Yeah, that's a silent killer. Patients think 'natural' means safe. Nope.
Jesse Ibarra
This is why medicine is a joke. You write a 2000-word treatise on blood thinners and still can't stop a 78-year-old grandma from taking ibuprofen for her arthritis. The system is broken. Doctors don't educate. Pharmacies don't warn. Patients don't listen. We're just throwing drugs at people and hoping they don't bleed out.
And don't even get me started on the $13,000 reversal agents. That's not medicine, that's a ransom note.
Randall Little
Fascinating. The real irony? We've got these life-saving reversal agents - idarucizumab, andexanet - but most rural ERs don't stock them because they're too expensive. Meanwhile, we're still using FFP like it's 1998. It's not incompetence. It's institutional cowardice. We know what works. We just won't pay for it.
Also, apixaban over warfarin? Absolutely. But only if you're not poor, elderly, or in a county with one pharmacist. The system fails the people who need it most.
Acacia Hendrix
The pharmacokinetic variability among DOACs is grossly underappreciated. Apixaban’s low renal excretion profile confers a superior safety index in the context of age-related glomerular filtration decline. Rivaroxaban, conversely, exhibits dose-dependent accumulation in CKD stages 3–4, rendering it pharmacologically untenable without stringent renal monitoring. The literature is unequivocal: renal function is not a variable - it is a determinant of therapeutic efficacy and hemorrhagic risk. Yet, we persist in treating anticoagulation as if it were a binary switch rather than a dynamic physiological equilibrium.
James Castner
There's a deeper truth here that nobody wants to admit: we treat anticoagulants like aspirin because we're afraid of the responsibility. We don't want to have the hard conversations. We don't want to sit with a patient and say, 'Your kidneys are failing, and this drug could kill you.' We just write the script and move on.
But here's the thing - medicine isn't about avoiding risk. It's about managing it with wisdom. Every time we skip a creatinine check, we're gambling with someone's life. And the cost isn't just dollars - it's dignity. It's the silence of a family who lost their parent because we were too busy to look at the lab report.
We need to stop treating patients like data points. We need to treat them like people. And that means slowing down. Checking labs. Asking about ginkgo. Knowing when to say no to the NSAID. That’s not just good medicine. That’s moral medicine.
Adam Rivera
My grandma’s on apixaban and I made sure her doc checked her CrCl before she started. She’s 82, weighs 55kg, and they gave her the 5mg dose at first. I caught it. She’s on 2.5mg now. I’m not a doctor, but I read. And I care.
Also, she stopped taking garlic supplements after I told her. No more ‘natural remedies’ unless we talk to the pharmacist first.
Rosalee Vanness
I’ve been caring for my dad since he had that GI bleed on rivaroxaban. We almost lost him. The hospital gave him andexanet - saved his life. But here’s what no one tells you: after you survive a bleed on a DOAC, you’re never the same. You’re scared to take a shower, scared to walk on the stairs, scared to sneeze too hard.
But here’s the good part - we restarted him on apixaban at 2.5mg, got his kidney numbers stable, and now he’s walking his dog every morning. It’s not perfect. It’s not easy. But it’s possible. You just have to be the advocate. Even if you’re not a doctor. Even if you’re just a kid who googled 'DOAC reversal agents' at 2 a.m.
Don’t let anyone make you feel like your voice doesn’t matter. You’re the one who notices the missed dose. You’re the one who remembers the ginkgo. You’re the one who says, 'Wait - is this right?'
Keep saying it.
lucy cooke
We are all just atoms dancing on the edge of a clot. The body is a temple, yes - but also a battlefield. And anticoagulants? They are the sword and the shield, wielded by hands too tired to hold them properly. We have the tools to reverse death - but we lack the humility to use them before it’s too late.
Apixaban is not a drug. It is a mirror. It reflects our neglect. Our haste. Our refusal to see the old man as a person, not a code in the EMR.
And yet… we still reach for it. Because life is worth fighting for. Even if we’re doing it wrong.
Trevor Davis
Just wanted to say thanks for writing this. My mom’s on warfarin and I used to think the INR checks were overkill. Now I know better. We do them every 4 weeks. She’s 79. No NSAIDs. No ginkgo. No excuses. We got lucky - she’s been stable for 2 years. But I know how thin that line is.
Also, I just told my cousin to stop taking turmeric with his blood thinner. He yelled at me. But I didn’t care. Better mad than dead.