Asthma & COPD Medication Interaction Checker
Check Your Medication Safety
Results
When you’re managing asthma or COPD, your inhaler isn’t the only thing that affects your breathing. Many of the medications you take for other conditions-pain relievers, sleep aids, even common cold remedies-can quietly make your lungs work harder or even trigger a dangerous flare-up. This isn’t theoretical. Real people are ending up in emergency rooms because they didn’t know a simple over-the-counter pill could interact with their daily inhaler.
Let’s be clear: asthma and COPD medications save lives. But when mixed with the wrong other drugs, they can turn into silent threats. The World Health Organization estimates over 470 million people worldwide live with one or both of these conditions. That means millions are at risk of harmful interactions, often without even realizing it.
What Medications Are You Really Taking?
Most people think of asthma and COPD meds as just inhalers: blue rescue inhalers, brown preventer inhalers, maybe a nebulizer. But treatment often includes more. Long-acting beta-agonists (LABAs) like formoterol or salmeterol, long-acting muscarinic antagonists (LAMAs) like tiotropium or glycopyrrolate, and inhaled corticosteroids are the backbone of daily management. Newer options like ensifentrine-a dual PDE3/4 inhibitor-have shown stronger bronchodilation when paired with LAMAs, but not with SABAs like albuterol. That matters because mixing the wrong combo doesn’t help-it can backfire.
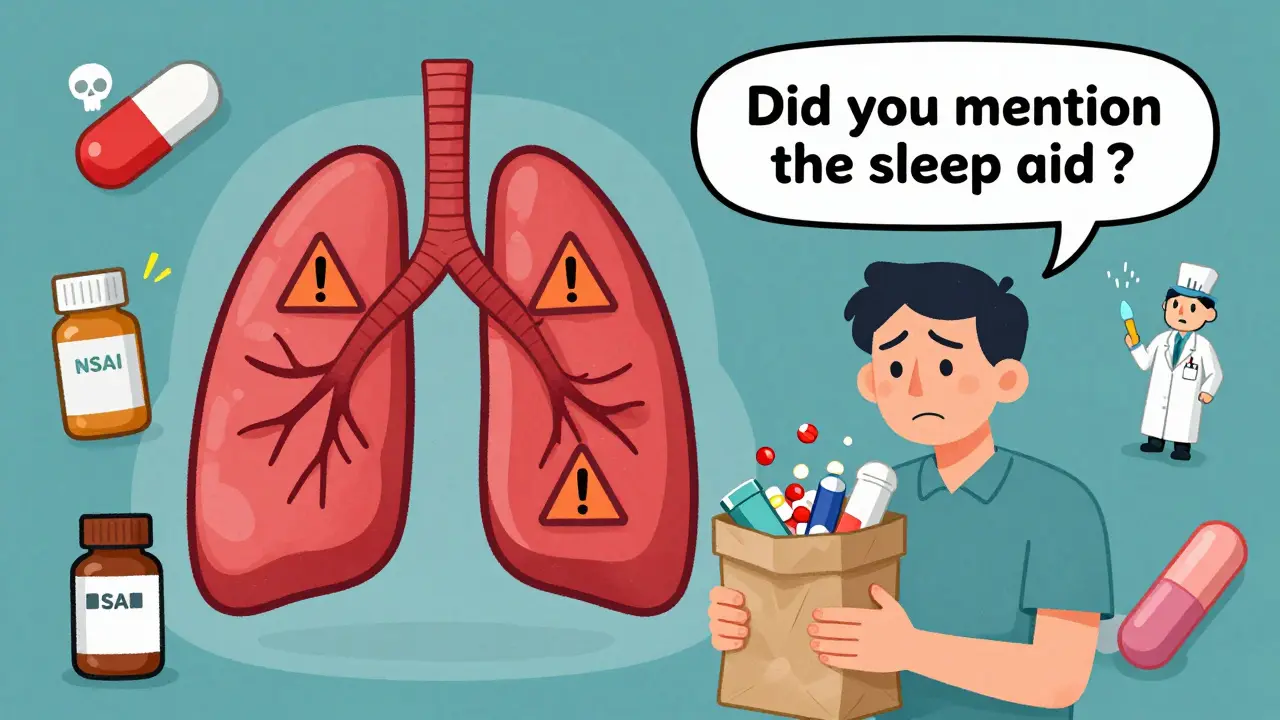
But here’s the problem: patients rarely think to mention every pill, patch, or supplement they take. A 2023 study in the Journal of the American Pharmacists Association found that clinical pharmacists reviewing full medication lists reduced dangerous combinations by 43% in just 12 months. Why? Because people forget-or don’t realize-that their arthritis painkiller, sleep aid, or bladder medication might be quietly working against their lung health.
The Hidden Dangers: Opioids and Benzodiazepines
If you have COPD, opioids are one of the most dangerous combinations you can take. Painkillers like oxycodone, hydrocodone, or even tramadol can slow your breathing. That’s bad enough on its own. But when you combine them with benzodiazepines-medications like diazepam (Valium) or lorazepam (Ativan)-the risk of life-threatening respiratory depression jumps by 300%, according to LPt Medical’s 2023 analysis. One Reddit user, “COPDSurvivor87,” described an oxygen saturation drop to 82% after mixing prescribed oxycodone with diphenhydramine (Benadryl). That’s not an outlier. The FDA’s Adverse Event Reporting System shows 17% of opioid-related hospitalizations in COPD patients involve this exact combo.
It’s not just prescription drugs. Over-the-counter sleep aids often contain diphenhydramine or doxylamine-both anticholinergics. When combined with a LAMA inhaler like tiotropium, they don’t just add up-they multiply. That’s why the European Respiratory Society warns of a 28% increased risk of acute urinary retention in male COPD patients taking both. Dry mouth? Constipation? Those are the mild signs. Slowed breathing? That’s the real danger.
Why Beta-Blockers Can Be a Silent Killer for Asthma
If you have asthma, avoid nonselective beta-blockers like propranolol or nadolol. These drugs are often prescribed for high blood pressure or heart rhythm issues, but they block the same receptors in your lungs that your rescue inhaler (albuterol) needs to open your airways. The result? Severe bronchospasm. Studies show these drugs can reduce FEV1 (a key measure of lung function) by 15-25% in sensitive individuals.
But not all beta-blockers are off-limits. Selective ones like metoprolol or bisoprolol are generally safe for mild to moderate asthma, with only 2-5% of patients experiencing symptoms. The 2021 BLOCK-COPD trial even showed a 14% reduction in exacerbations when COPD patients with heart disease switched from nonselective to selective beta-blockers. The key? Your doctor needs to know your full history. Don’t assume your cardiologist is aware of your asthma meds-and don’t assume your pulmonologist knows about your heart pills.

NSAIDs: The Painkiller That Can Trigger an Attack
Take ibuprofen or naproxen for a headache? If you have asthma, especially with nasal polyps or chronic sinusitis, you’re at risk. About 10% of adult asthma patients react to NSAIDs, with symptoms like wheezing, chest tightness, or full-blown asthma attacks occurring within 30 to 120 minutes. A Reddit user named “BreathingHard2020” had a severe attack after taking ibuprofen-no prior history of reactions. That’s common. Asthma + Lung UK’s 2023 survey found that 31% of respondents had experienced breathing trouble from non-respiratory medications, and 68% didn’t connect the dots until it happened.
Acetaminophen (paracetamol) is usually a safer alternative for pain relief in asthma patients. But even then, don’t assume safety. Some combination cold remedies contain NSAIDs, decongestants, or antihistamines-all of which can interfere with your lung meds. Always read the full ingredient list.
Anticholinergic Overload: More Isn’t Better
LAMAs like tiotropium, aclidinium, and umeclidinium are powerful tools for COPD. But they’re anticholinergics-meaning they block acetylcholine, a nerve signal that tightens airways. That’s good for lungs. But if you’re also taking oxybutynin for an overactive bladder, diphenhydramine for allergies, amitriptyline for depression, or benztropine for Parkinson’s, you’re stacking anticholinergic effects.
The result? Dry mouth, constipation, blurred vision, urinary retention, and confusion. In older adults, these aren’t just annoyances-they’re red flags for worsening lung function. The Asthma + Lung UK Inhaler Guide explicitly warns against combining inhalers with these oral anticholinergics. One 2023 study found that patients taking two or more anticholinergic drugs had a 32% higher chance of hospitalization for respiratory issues than those on one.

Antibiotics and Antifungals: The Silent Interferers
Clarifying your medication list isn’t just about what you take for your lungs-it’s about what you take for everything else. Antibiotics like clarithromycin and erythromycin inhibit the CYP3A4 liver enzyme, which breaks down many COPD and asthma drugs. This causes levels of your inhaler medication to build up dangerously high, increasing side effects like tremors, rapid heartbeat, or even heart rhythm problems.
The same goes for antifungals like ketoconazole or itraconazole. These are often prescribed for fungal infections, but they can spike the concentration of inhaled corticosteroids in your bloodstream. The American Lung Association warns that many patients don’t realize these drugs-even taken for a week-can cause systemic side effects like adrenal suppression or bone loss over time.
What You Can Do Right Now
You don’t need to be a medical expert to protect yourself. Here’s what works:
- Keep a real-time medication list. Write down every pill, patch, inhaler, supplement, and OTC drug-including dosage and why you take it. Update it after every doctor visit.
- Bring everything to appointments. The “brown bag test” isn’t a joke. Take all your meds in a bag to your pulmonologist, GP, or pharmacist. They’ll spot the red flags you miss.
- Ask two questions at every prescription: “Could this interact with my asthma or COPD meds?” and “Is there a safer alternative?”
- Use digital tools. The COPD Medication Safety App (launched in 2023) checks 95% of common drugs for interactions. It’s free, simple, and works offline.
- Know your warning signs. Sudden shortness of breath, increased wheezing, confusion, dizziness, or urinary retention after starting a new drug? That’s not coincidence. Call your doctor.
Electronic health records now include respiratory-specific interaction alerts. But they’re only as good as the data you give them. If you don’t tell your doctor about your daily antihistamine or your weekend painkiller, the system won’t catch it.
It’s Not Just About Inhalers
The biggest mistake patients make? Thinking their respiratory meds exist in isolation. They don’t. Your lungs are connected to your heart, your liver, your bladder, your nervous system. A drug that seems unrelated-like a bladder pill or a sleep aid-can be the missing link in your worsening symptoms.
One patient told the COPD Foundation, “I thought my breathing got worse because my COPD was getting worse. Turns out, it was the sleeping pill I started six months ago.” That’s the quiet truth behind most medication-related crises. It’s not about what you’re taking for your lungs. It’s about what you’re taking for everything else.
Respiratory disease management has come a long way. But safety still lags behind innovation. New drugs like ensifentrine show promise. But if you’re stacking anticholinergics or mixing opioids with sedatives, you’re undoing the benefits before they even start.
You’re not alone. Millions of people are managing complex medication regimens. The difference between staying well and ending up in the ER often comes down to one thing: awareness. And that starts with a simple list. A real conversation. And the courage to ask: Could this hurt me?
Can I take ibuprofen if I have asthma?
About 10% of adults with asthma, especially those with nasal polyps or chronic sinusitis, can have a severe reaction to ibuprofen and other NSAIDs. Symptoms include wheezing, chest tightness, or full asthma attacks within 30-120 minutes. Acetaminophen (paracetamol) is usually a safer alternative for pain relief. Always check with your doctor before using NSAIDs regularly.
Are beta-blockers safe for people with asthma?
Nonselective beta-blockers like propranolol and nadolol can trigger severe bronchospasm by blocking lung receptors and should be avoided. Selective beta-blockers like metoprolol or bisoprolol are generally safe for mild to moderate asthma, with only 2-5% of patients experiencing symptoms. The 2021 BLOCK-COPD trial showed that switching to metoprolol reduced COPD exacerbations by 14% in patients with heart disease. Always confirm with your pulmonologist and cardiologist before starting any beta-blocker.
Can I use Benadryl if I have COPD?
Diphenhydramine (Benadryl) is an anticholinergic and can worsen COPD by increasing mucus thickness and reducing lung clearance. When combined with LAMA inhalers like tiotropium, it raises the risk of urinary retention, confusion, and respiratory depression. Studies show a 28% higher chance of hospitalization for male COPD patients using both. Use non-sedating antihistamines like loratadine or cetirizine instead, and always discuss OTC options with your pharmacist.
Do antibiotics interact with asthma and COPD medications?
Yes. Antibiotics like clarithromycin and erythromycin inhibit the CYP3A4 enzyme, which can cause dangerous buildup of inhaled corticosteroids or LABAs in your bloodstream. This increases risks of tremors, rapid heartbeat, or adrenal suppression. Antifungals like ketoconazole have the same effect. Always tell your doctor you’re on respiratory meds before starting any new antibiotic or antifungal.
What’s the brown bag test and why should I do it?
The brown bag test means bringing all your medications-including prescriptions, over-the-counter drugs, vitamins, and supplements-to your doctor or pharmacist in a bag. This helps them spot dangerous interactions you might miss. A 2022 study showed that pharmacist-led reviews using this method reduced high-risk combinations by 43% in COPD patients. It’s simple, free, and could save your life.
Is there an app to check for medication interactions?
Yes. The COPD Medication Safety App, launched in 2023 by the COPD Foundation, checks interactions between 95% of commonly prescribed respiratory and non-respiratory medications. It works offline, is free to use, and alerts you to dangerous combos like opioids + anticholinergics or NSAIDs + asthma. It’s one of the most practical tools available for patients managing multiple medications.

Brett Pouser
Man, I wish I'd known this stuff years ago. My dad was on oxygen and took ibuprofen for his back pain-no one ever told him it could trigger a flare-up. He ended up in the ER twice before we figured it out. Now he uses acetaminophen and keeps a written list of everything. Simple. But life-changing.
Stop assuming your doctor knows your full med list. They don’t. You gotta be your own advocate.
Karianne Jackson
Benadryl is the worst. I took it for allergies and almost passed out. My lungs felt like they were wrapped in plastic. Never again. Just take Zyrtec. So much easier.
Lyle Whyatt
Let me tell you about the time I was on tiotropium and started taking oxybutynin for my bladder. Thought I was being smart-two prescriptions, two problems solved. Nope. Within weeks, I couldn’t pee, my mouth felt like the Sahara, and I was dizzy 24/7. Went to my pharmacist and he looked at me like I’d just admitted to stealing a car.
Turns out, I was stacking anticholinergics like a damn science experiment. My pulmonologist said I was lucky I didn’t end up in ICU. Now I only take one anticholinergic at a time, and I ask the pharmacist every single time I get a new script. Seriously, if you’re on a LAMA, don’t even think about OTC sleep aids. They’re not harmless. They’re landmines.
And don’t get me started on NSAIDs. I thought my wheezing after ibuprofen was just stress. Turns out, it was a full asthma attack. I’ve been on paracetamol since. No more guessing. No more ‘maybe.’ Just write it down. Bring it in. Ask the damn questions.
Also-yes, the COPD Medication Safety App is legit. I use it every time I pick up a new pill. It flagged a combo of clarithromycin and my inhaler. Saved me. Free. Offline. Works great. Download it. Use it. Your lungs will thank you.
And if you’re on beta-blockers? Don’t assume they’re safe. Ask if it’s selective. If they don’t know, get a second opinion. Your heart and lungs are connected. Treat them like it.
Tom Forwood
Y’all are overcomplicating this. Just bring your meds in a bag to your pharmacist. That’s it. No fancy apps, no memorizing drug names. Just dump everything on the counter and say ‘help me.’ They’ll catch what the docs miss.
Also-don’t take Benadryl if you have COPD. Period. Even if you think it’s ‘just for allergies.’ It’s not. It’s a slow poison for your lungs. Use loratadine. It’s cheap. It works. No drowsiness. No dry throat. No hospital trips.
And if your doc prescribes a new painkiller? Ask ‘will this mess with my inhaler?’ If they look confused, go somewhere else. Your lungs aren’t optional.
Joseph Charles Colin
From a clinical pharmacology standpoint, the CYP3A4 inhibition by macrolide antibiotics (clarithromycin, erythromycin) and azole antifungals (ketoconazole, itraconazole) significantly elevates plasma concentrations of inhaled corticosteroids (e.g., fluticasone, budesonide) and LABAs (e.g., salmeterol, formoterol). This can lead to systemic glucocorticoid excess-manifesting as adrenal suppression, osteoporosis, hyperglycemia, and QT prolongation. The half-life of these inhaled agents can extend from 8–12 hours to >24 hours under enzyme inhibition.
Similarly, dual anticholinergic burden (e.g., tiotropium + oxybutynin) increases muscarinic receptor occupancy beyond therapeutic thresholds, elevating risk of urinary retention (OR 2.1, 95% CI 1.6–2.8) and cognitive impairment in elderly COPD patients. The European Respiratory Society’s 2022 guidelines explicitly recommend avoiding concomitant use.
Pharmacogenomic variability in CYP3A4 activity (e.g., *1B/*22 haplotypes) further modulates risk, necessitating individualized risk stratification. Digital tools like the COPD Medication Safety App are valuable but should supplement-not replace-clinical decision-making.
Elan Ricarte
So let me get this straight-you’re telling me people are dying because they didn’t read the damn label? Like, what the fuck? You take a sleeping pill because you’re tired, and suddenly you’re choking on your own breath? That’s not a medical mystery. That’s negligence wrapped in a prescription bottle.
And you know who’s to blame? Doctors. They write scripts like they’re handing out candy. ‘Here, take this for sleep.’ ‘Here, take this for pain.’ No context. No warning. No ‘hey, your lungs are already on life support.’
And don’t even get me started on ‘selective’ beta-blockers. Yeah, sure, metoprolol is ‘safe.’ Until it isn’t. You think your cardiologist actually knows you’re on a LAMA? Nah. They’re too busy checking off boxes for their bonus. You’re the only one who gives a shit. So stop waiting for permission. Start asking questions. Bring your meds. Read the fucking insert. If you’re not paranoid, you’re not paying attention.
And if you’re still using Benadryl? You’re not a patient-you’re a walking emergency.
Chelsea Deflyss
why do people not just ask their drs? like its not that hard. i had a friend who took ibuprofen and ended up in the er and she was like ‘i didnt think it would do that’... honey, if it says ‘may cause bronchospasm’ on the bottle, maybe dont take it. lol.
Scott Conner
Does this app work with non-US meds? I’m on a Canadian prescription for tiotropium and my OTC stuff is all different. Just wondering if it’s worth downloading.
Alex Ogle
I’ve been living with COPD for 12 years. I used to think my worsening breathlessness was just the disease getting worse. Turns out? It was the melatonin I started taking after my mom passed. Didn’t even realize it had diphenhydramine in it. Took me six months to connect the dots.
Now I only take one OTC thing at a time. And I check every bottle like it’s a bomb. I don’t trust labels. I don’t trust doctors. I don’t trust ‘it’s just a little something.’
The truth? Your lungs don’t care if you meant well. They only care if you did the right thing. And the right thing is always-always-checking before you take something new. Even if it’s just a vitamin. Especially if it’s just a vitamin.
Brandon Osborne
OMG I CAN’T BELIEVE PEOPLE ARE STILL DOING THIS. I HAD A COUSIN WHO TOOK OXYCODONE AND BENADRYL FOR ‘SLEEP’ AND SHE ALMOST DIED. HER O2 DROPPED TO 78%. SHE WAS IN A COMA FOR THREE DAYS. AND NOW SHE’S LIKE ‘I’LL JUST USE A DIFFERENT SLEEP AID.’ NO. YOU’LL JUST DIE AGAIN.
THIS ISN’T A ‘MAYBE.’ THIS ISN’T A ‘MIGHT.’ THIS IS A DEADLY COMBO. IF YOU’RE DOING THIS, YOU’RE A LIABILITY TO YOURSELF AND EVERYONE AROUND YOU.
STOP BEING LAZY. STOP BEING STUBBORN. READ THE LABEL. TALK TO YOUR PHARMACIST. OR JUST STOP TAKING STUFF YOU DON’T UNDERSTAND.
WE’RE NOT HERE TO BABY YOU. WE’RE HERE TO SAVE LIVES. AND YOURS ISN’T ONE OF THEM IF YOU KEEP IGNORING THIS.
Marie Fontaine
Yessss! I use the COPD app every week!! 🙌 I even showed my mom and she’s been using it too. She’s 71 and on 8 meds-now she checks every new thing before she takes it. No more guessing! 💪
Also-switched from Benadryl to Claritin and my breathing improved in a week. I wish I knew sooner 😭
PS: brown bag test is a game changer. My pharmacist caught a dangerous combo I had no clue about. She’s basically my superhero. ❤️
Andy Cortez
Oh wow, so the app works offline? That’s the only reason I’d use it. My data’s trash. But yeah, I still think people are being too nice about this. You don’t need an app. You need a brain. And if you’re still mixing opioids with sleep aids? You’re not sick-you’re just dumb. No offense. But if your lungs are this fragile, maybe don’t treat your meds like a buffet.
Lyle Whyatt
Yeah, I saw your comment about the app. I’ve been using it since last fall. It saved me when my doc prescribed a new antibiotic. The app flagged it-turns out it was a CYP3A4 inhibitor. I called my pharmacist and he said, ‘Thank god you checked.’
And to the person who said ‘just ask your doctor’-I get it. But half the time, my pulmonologist doesn’t even know what my cardiologist prescribed. And my cardiologist doesn’t know I’m on tiotropium. So who’s left? Me. I’m the only one holding the whole damn list.
Don’t wait for someone else to protect you. You’re the only one who can.