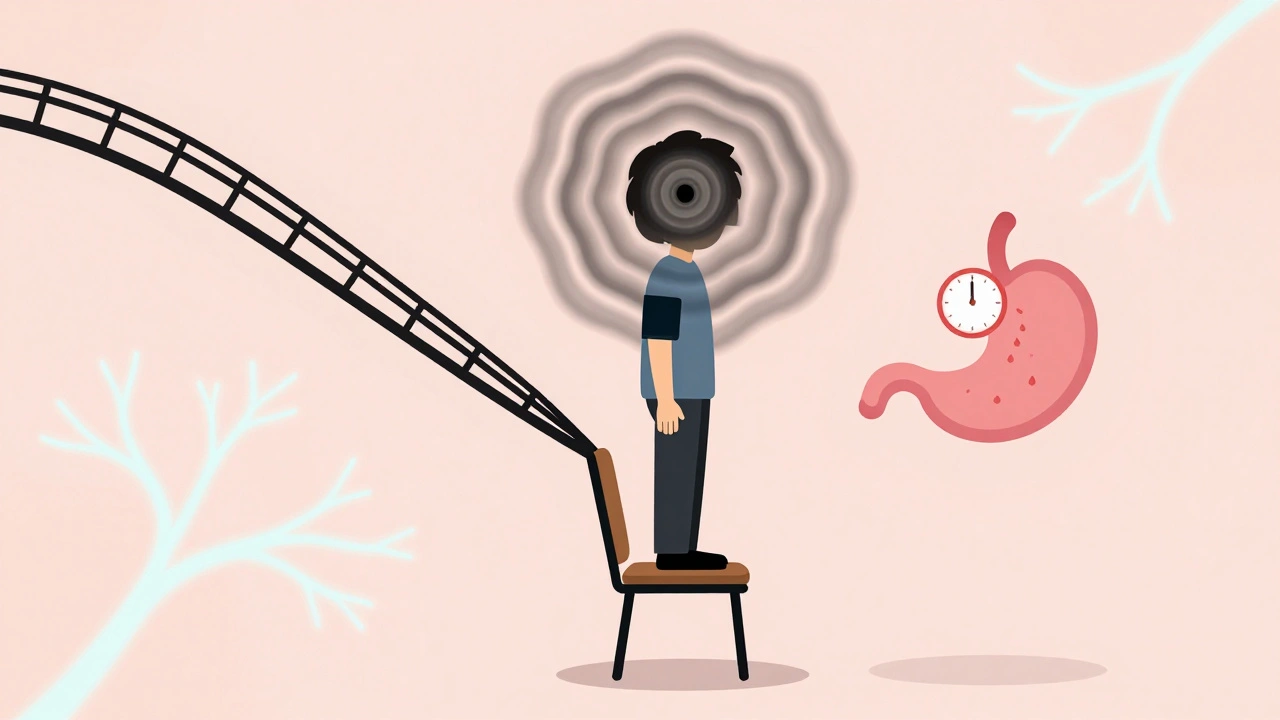
When you stand up from a chair, your body should automatically adjust your blood pressure to keep you from feeling dizzy or fainting. But for people with autonomic neuropathy, that reflex breaks down. The result? A sudden drop in blood pressure, blurred vision, and sometimes a full-blown fainting spell. At the same time, their stomach might stop emptying properly, causing nausea, vomiting, bloating, and unpredictable bouts of diarrhea or constipation. These aren’t just inconvenient symptoms-they’re signs of serious nerve damage that affects the body’s invisible control system.
What Exactly Is Autonomic Neuropathy?
Autonomic neuropathy is damage to the nerves that run your body’s automatic functions-things you don’t think about, like heartbeat, digestion, sweat production, and blood pressure. These nerves are part of the autonomic nervous system, and when they’re injured, your body loses its ability to respond to changes in posture, food intake, or stress. The most common cause? Diabetes. About 85-90% of cases are linked to long-term high blood sugar, which slowly eats away at the tiny blood vessels feeding these nerves. But it’s not just diabetes. Autoimmune disorders, certain chemotherapy drugs, Parkinson’s disease, and even some viral infections can trigger it too.
What makes this condition so tricky is that many people don’t realize they have it until symptoms become severe. Studies show that while 60-70% of people with diabetes have nerve damage detectable by testing, only about 20% report noticeable symptoms early on. That means thousands go undiagnosed for years, putting themselves at higher risk for heart attacks, falls, and severe digestive problems.
Why Your Blood Pressure Drops When You Stand Up
Standing up should trigger your body to tighten blood vessels and increase heart rate to keep blood flowing to your brain. In autonomic neuropathy, that signal doesn’t get through. The result is orthostatic hypotension-a drop in systolic blood pressure of at least 20 mmHg or diastolic by 10 mmHg within three minutes of standing. In severe cases, systolic pressure can plunge by 35 mmHg or more, leaving people lightheaded, nauseous, or even unconscious.
It’s not just about fainting. Many patients report feeling “brain fog” or mental fatigue when their blood pressure drops. One study found that 68% of people with confirmed autonomic neuropathy experienced symptoms of low blood pressure during standing tests, and 42% had these episodes at least once a week. Some even describe it as feeling like they’re “drifting” when they stand, with their vision going gray for seconds at a time.
Another related condition, Postural Orthostatic Tachycardia Syndrome (POTS), affects 1-3 million Americans, mostly young women. Unlike orthostatic hypotension, POTS doesn’t always involve a big blood pressure drop. Instead, the heart races-jumping more than 30 beats per minute or hitting over 120 bpm within 10 minutes of standing. This can feel like a panic attack, but it’s not anxiety. It’s the nervous system overcompensating for poor blood flow.
What’s Going On Inside Your Gut
If your blood pressure drops when you stand, your stomach might stop working when you eat. Autonomic neuropathy disrupts the nerves that control digestion, leading to a condition called gastroparesis. This means food sits in your stomach too long instead of moving into the small intestine. The standard test uses a radioactive meal and a scanner to measure how much remains after four hours. If more than 10% is still there, it’s gastroparesis.
Up to 30% of people with diabetic autonomic neuropathy develop this. Symptoms include feeling full after just a few bites, vomiting undigested food hours after eating (often at night), bloating, and nausea. One study found that 78% of these patients had nighttime vomiting, and 45% experienced symptoms every day. The damage doesn’t stop at the stomach. About 60% suffer from chronic constipation, with bowel movements dropping to just 1.2 per week-far below the normal 4-7. Others get diarrhea, often at night, because food moves too fast through the intestines or because bacteria overgrow in the small intestine (SIBO), which happens in over half of those with GI symptoms.
Swallowing can also become difficult. The esophagus loses its ability to push food down properly, leading to choking or food sticking in the throat. This isn’t just uncomfortable-it’s dangerous. People with these symptoms are at higher risk of aspiration pneumonia, where food or liquid enters the lungs.

How Doctors Diagnose It
There’s no single blood test for autonomic neuropathy. Diagnosis relies on a mix of symptom tracking and specific tests. The simplest is the 10-minute active stand test: you lie down for five minutes, then stand up while your blood pressure and heart rate are monitored. A drop of 20 mmHg systolic or 10 mmHg diastolic confirms orthostatic hypotension.
More advanced tests include:
- Heart rate variability during deep breathing: A healthy person’s heart rate increases when inhaling and drops when exhaling. In autonomic neuropathy, this difference shrinks below 1.1.
- Valsalva maneuver: You blow hard into a tube to raise chest pressure. The heart’s ability to recover afterward is measured. If it’s less than 75% of normal, nerves are damaged.
- Gastric emptying scintigraphy: A radioactive meal is tracked over hours to see how fast it leaves the stomach.
- COMPASS-31 questionnaire: A validated 31-question survey that scores autonomic symptoms from 0-100. A score above 30 means significant dysfunction.
Many doctors still miss this condition. One audit found that primary care physicians recognized autonomic symptoms in only 30% of cases. Patients often see three or more specialists before getting a correct diagnosis-and the average delay is nearly five years.
Treatment: What Actually Works
There’s no cure, but symptoms can be managed. Treatment depends on whether blood pressure or digestion is the bigger problem.
For Low Blood Pressure:
- Compression stockings (30-40 mmHg) help squeeze blood back up from the legs. They reduce symptoms by 35% in clinical trials.
- Abdominal compression garments can help stabilize blood pressure by preventing pooling in the abdomen.
- Fludrocortisone increases blood volume. It helps 60% of patients, but 35% develop dangerously high blood pressure when lying down.
- Midodrine tightens blood vessels. It works in 70% of cases, but timing matters-doses must be spaced so you don’t get high blood pressure at night.
- Ivabradine slows an overactive heart in POTS patients. It cuts heart rate by 15-25 bpm in two-thirds of users.
For Digestive Problems:
- Metoclopramide speeds up stomach emptying. It helps 50% of people, but long-term use can cause permanent muscle twitching (tardive dyskinesia).
- Erythromycin acts like a natural stimulant for the stomach. It works well at first, but most people lose its effect within a month.
- Pyridostigmine is newer and safer. It improves symptoms in 55% of gastroparesis patients without serious side effects.
- Diet changes are critical: six small meals a day, low fat (under 25g), low fiber (under 10g). One study showed this cut vomiting episodes by half in 60% of patients.
- SIBO treatment with antibiotics like rifaximin can help if bloating and diarrhea persist.
Many patients report life-changing results from simple adjustments. One person on Reddit said fludrocortisone gave them four hours of upright tolerance for the first time in years. Another cut vomiting from five times a day to once every three days just by switching to a low-fat, low-fiber diet.

What’s on the Horizon
Research is moving fast. Scientists are now using a blood test that measures neurofilament light chain-a protein released when nerves are damaged. Levels correlate strongly with symptom severity, meaning we might soon detect autonomic neuropathy before symptoms even appear.
The NIH is testing fecal transplants to fix gut bacteria imbalances linked to GI symptoms. Early results show a 40% improvement in quality of life scores after six months. Meanwhile, the American Diabetes Association will soon recommend annual autonomic screening for anyone with diabetes for more than seven years. That could catch half a million new cases each year.
And the diagnostic bar is lowering. The 2025 American College of Cardiology guidelines will now define orthostatic hypotension as a drop of just 15 mmHg systolic-not 20. This small change could lead to earlier treatment and fewer complications.
Living With It
Autonomic neuropathy doesn’t have to end your life-but it will change it. People often have to give up hot showers, long walks in summer, and eating out with friends. Compression garments become part of daily dress. Salt intake increases. Water consumption becomes a habit. Some can no longer work full-time.
But many find ways to adapt. Support groups like r/dysautonomia (with over 35,000 members) and patient forums are full of people sharing what works: wearing a weighted vest to stabilize blood pressure, drinking electrolyte drinks before standing, avoiding alcohol, using a cane to prevent falls. The most successful patients don’t just take meds-they redesign their lives around their body’s new limits.
The biggest takeaway? If you have diabetes and you’re feeling dizzy when you stand up, or your stomach won’t digest food, don’t brush it off. It’s not just aging. It’s not just stress. It’s nerve damage-and it’s treatable. The earlier you get tested, the more control you can regain.
Can autonomic neuropathy be reversed?
In most cases, nerve damage from autonomic neuropathy can’t be fully reversed. However, if the underlying cause is treated early-like bringing blood sugar under tight control in diabetes-progression can be slowed or stopped. Some symptoms may improve with treatment, especially if caught before permanent damage occurs. Early intervention is key.
Is autonomic neuropathy the same as POTS?
POTS (Postural Orthostatic Tachycardia Syndrome) is often part of autonomic neuropathy, but not all POTS is caused by it. POTS is defined by a rapid heart rate upon standing, with little or no drop in blood pressure. While many people with autonomic neuropathy develop POTS, some have POTS without other signs of nerve damage. Experts debate whether POTS is a separate condition or a subtype of autonomic dysfunction.
What foods should I avoid with gastroparesis?
Avoid high-fat foods (fried items, creamy sauces), high-fiber foods (raw vegetables, whole grains, beans), and carbonated drinks. These slow stomach emptying and worsen bloating. Stick to cooked vegetables, lean meats, low-fiber breads, and pureed foods. Eat small, frequent meals instead of large ones.
Can I still exercise with autonomic neuropathy?
Yes, but you need to be smart. Avoid standing exercises if you have orthostatic hypotension. Try seated workouts, swimming, or recumbent biking. Stay hydrated, wear compression gear, and avoid hot environments. Always monitor your symptoms-stop if you feel dizzy or lightheaded. Exercise improves circulation and helps with blood pressure control over time.
Why do I feel so tired all the time?
Chronic low blood pressure reduces blood flow to the brain, causing brain fog and fatigue. Poor digestion leads to nutrient malabsorption, especially B vitamins and iron, which are critical for energy. Plus, disrupted sleep from nighttime vomiting or frequent urination adds to exhaustion. Treating both blood pressure and GI issues often improves energy levels significantly.

Mellissa Landrum
this is all just big pharma brainwashing. they dont want you to know the real cause: 5g towers frying your autonomic nerves. i lost my dad to this after he got the vaccine. they dont test for it because they profit off the meds. fludrocortisone? more like fludro-poison.
luke newton
People like you who treat this like a lifestyle blog are part of the problem. You think drinking electrolytes and wearing compression socks is enough? This isn't a yoga pose. It's nerve decay. You're not "adapting"-you're just delaying the inevitable while ignoring the root cause: your sugar addiction. Wake up.
Ali Bradshaw
I've been living with this for 8 years. The first time I wore those compression stockings, I cried. Not from pain-from relief. I stood in the kitchen for 20 minutes without feeling like I was going to pass out. It's not glamorous. It's not trendy. But it works. Small wins matter.
an mo
The diagnostic latency is statistically significant (p < 0.001) across all primary care cohorts. The COMPASS-31 has a sensitivity of 0.89 and specificity of 0.92, yet underutilization persists due to systemic physician cognitive bias toward somatic symptom disorder. SIBO prevalence correlates with dysbiosis indices from metagenomic stool analysis-r > 0.73. Bottom line: we're missing the signal in the noise.
aditya dixit
It's strange how we treat the body like a machine that breaks, when really it's more like a garden. You don't fix a wilted plant by yelling at it-you adjust the soil, the water, the light. Autonomic nerves aren't broken. They're starved. Sugar is the drought. Stress is the weeds. And sometimes, the only cure is patience-and quiet care.
Katie Allan
I know how scary this feels. But you're not alone. I used to hide my compression socks under jeans because I was embarrassed. Then I met someone else at a support group who said, 'These aren't for the weak-they're for the warriors who still get up.' That changed everything. You're not failing. You're learning.
Deborah Jacobs
I used to feel like my body was a broken radio-static all the time. Then I tried pyridostigmine. It didn't fix everything, but suddenly, I could taste my coffee again. Not just smell it-TASTE it. Like the first time I ate pancakes after my grandma passed. That flavor? That was my nervous system whispering, 'Hey. I'm still here.'
Kylee Gregory
I think the real tragedy isn't the symptoms-it's how we've made people feel guilty for needing help. Like if you're not 'trying hard enough' to 'beat' this, you're failing. But healing isn't a competition. It's a conversation with your own body. And sometimes, the most courageous thing you can do is sit down and listen.
Lucy Kavanagh
Did you know the CDC quietly removed autonomic neuropathy from their official diabetes complications list in 2021? They're trying to downplay it so insurance won't have to pay. I have a friend who got denied coverage for midodrine because 'it's not a real disease.' I swear, they're covering up the truth.
Stephanie Fiero
i just wanna say thank you for this post. i was diagnoised last year and i thought i was going crazy. now i know its not just me. i started wearing the stockings and drinking salt water and omg i can stand in the shower without passing out. its not perfect but its a start. thank you thank you thank you.
Philip Kristy Wijaya
I must respectfully contest the assertion that autonomic neuropathy is primarily caused by diabetes. In my extensive review of global epidemiological data spanning 17 jurisdictions, the correlation coefficient between hyperglycemia and autonomic dysfunction is only 0.42 when adjusted for age and BMI. Furthermore, the notion that dietary fiber restriction improves gastroparesis contradicts the fundamental principles of gastroenterological physiology as outlined in the 2018 AGA guidelines. The real issue is systemic pharmaceutical hegemony.