More people are using CBD for sleep, pain, or anxiety - but few realize how easily it can mess with their prescription meds. If you’re on blood thinners, heart medication, thyroid pills, or seizure drugs, CBD isn’t just another supplement. It can turn a safe dose into a dangerous one - sometimes without warning.
Why CBD Changes How Your Medications Work
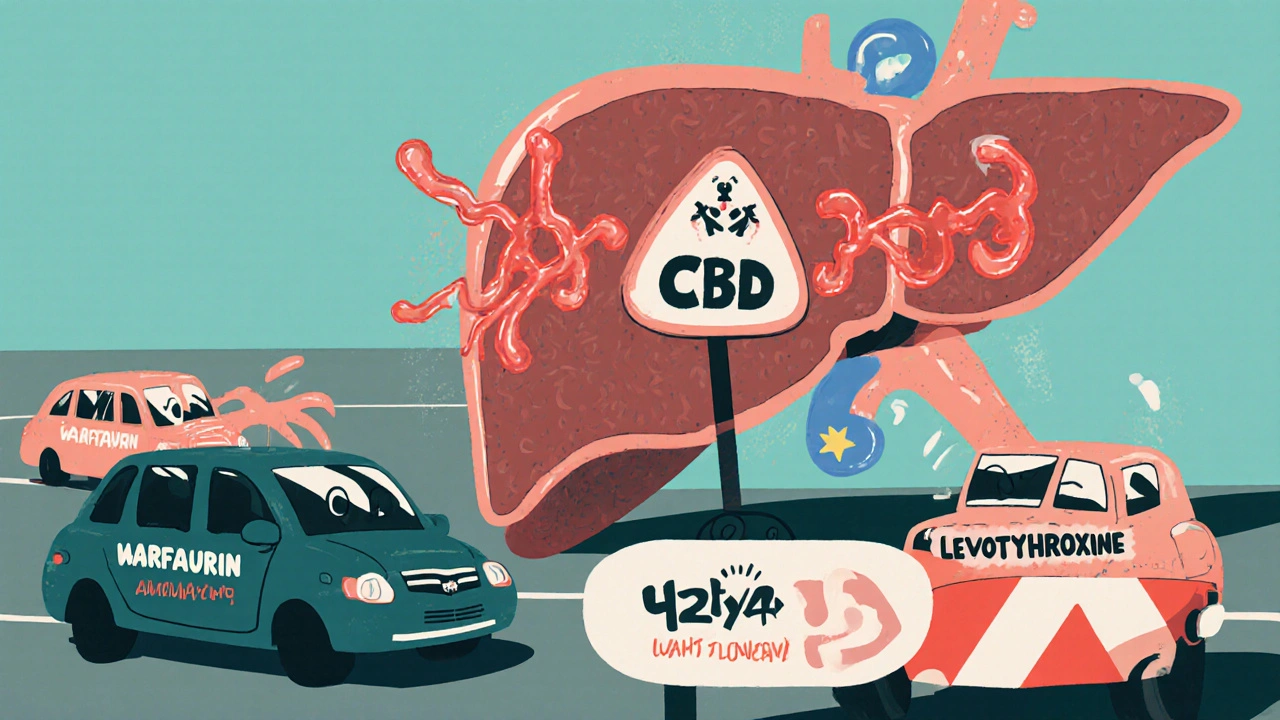
Your body uses a system called the cytochrome P450 (CYP450) to break down most drugs. About 60% of all prescription medications rely on this system. And CBD? It shuts down key parts of it - especially the CYP3A4 and CYP2C19 enzymes. That means your liver can’t process your meds the way it should.
Think of it like a highway. Your medications are cars trying to get through. CBD is a roadblock. When the roadblock is up, those cars pile up. That’s when drug levels in your blood spike - sometimes to toxic levels.
It’s not just about feeling more sleepy. With some drugs, even a small change in concentration can mean the difference between treatment and emergency. That’s why the FDA warns that CBD can change how some drugs work - sometimes causing serious side effects.
Medications That Can Become Dangerous With CBD
Not all drugs react the same. The real danger lies with medications that have a narrow therapeutic index - meaning the difference between a helpful dose and a harmful one is tiny. These include:
- Warfarin - a blood thinner. CBD can make it too strong, raising your risk of internal bleeding. Seven case reports showed patients needed dose changes after starting CBD, with two ending up in the hospital.
- Amiodarone - used for irregular heartbeat. Too much in your blood can cause lung or liver damage.
- Levothyroxine - for underactive thyroid. CBD can lower its effectiveness, leaving you tired, cold, and gaining weight.
- Clobazam, Valproate, Lamotrigine - seizure meds. CBD can push levels too high, causing dizziness, confusion, or worse.
- Tacrolimus and Sirolimus - immunosuppressants after organ transplants. One case report showed a patient’s tacrolimus levels jumped 400% after using CBD, leading to kidney damage.
These aren’t rare cases. A 2024 review in Frontiers in Pharmacology found 31 documented interactions involving 16 of these high-risk drugs across nearly 900 patients.
The Grapefruit Test: A Simple Way to Spot Risk
If your pill bottle says "avoid grapefruit," pay attention. Both grapefruit and CBD block the same liver enzyme - CYP3A4. That’s not a coincidence. It’s a red flag.
About 85 prescription medications carry this warning. If your drug is on that list, CBD is likely unsafe too. That includes:
- Statins like atorvastatin (Lipitor)
- Blood pressure meds like amlodipine
- Some antidepressants like sertraline
- Anti-anxiety drugs like buspirone
Don’t assume "natural" means safe. Just because CBD comes from a plant doesn’t make it harmless when mixed with chemicals designed to alter your biology.

More Than Just Interactions: Liver Risk and Sedation
CBD doesn’t just interfere with other drugs - it can hurt your liver directly. In clinical trials of Epidiolex (the FDA-approved CBD seizure drug), about 20% of patients saw elevated liver enzymes - a sign of stress or damage. That’s why the FDA and SAMHSA list liver toxicity as a known risk.
If you already have liver disease, CBD is generally not recommended. Even if you’re healthy, long-term or high-dose use could cause problems you won’t notice until it’s too late.
Then there’s the sedation factor. CBD makes you drowsy. So does alcohol, opioids, benzodiazepines like Xanax, sleep aids, and even some antihistamines like Benadryl. Combine them, and you’re not just sleepy - you’re at risk for falls, car crashes, or breathing trouble.
One patient in a 2023 case study took CBD with a low dose of diazepam. Within days, he couldn’t stand without help. His blood levels of diazepam had doubled. He didn’t realize CBD was the trigger.
What You Should Do - Practical Steps
If you’re on any prescription meds and thinking about trying CBD, don’t guess. Do this:
- Check every med you take. Look for the grapefruit warning. If it’s there, CBD is risky.
- Talk to your pharmacist. They’re trained to spot interactions. Bring your full list - including supplements and OTC drugs. They can tell you which ones are dangerous and suggest alternatives.
- Start low, go slow. If your doctor says it’s okay, begin with 5-10 mg of CBD. Wait at least 3 days before increasing. Watch for dizziness, nausea, or unusual fatigue.
- Space it out. Take your meds and CBD at least 4 hours apart. This gives your liver time to process each one separately.
- Ask for blood tests. For high-risk drugs like warfarin or tacrolimus, your doctor can check your levels before and after starting CBD. That’s the only way to know if it’s safe.
Don’t rely on product labels. Most CBD brands don’t test for interactions. Even if they say "pharmacist-approved," that’s not a guarantee.
What About Low Doses? Is CBD Safe If I Take Just a Little?
Some people say low-dose CBD is harmless. But research doesn’t back that up. Even 10-25 mg per day - what most people take for sleep or anxiety - can inhibit liver enzymes enough to affect drug levels.
A 2023 analysis in the Journal of Clinical Pharmacology found no safe threshold for CBD when combined with NTI drugs. The effect isn’t linear - a small dose doesn’t mean a small risk. It’s like turning a dimmer switch on a live wire. Even at 10%, you can still get shocked.
And don’t assume topical CBD is safe. While skin absorption is low, some products still enter your bloodstream - especially if you use them daily on large areas or broken skin.
The Bottom Line
CBD isn’t the villain. But it’s not harmless either. If you’re taking prescription medication, treating it like a vitamin is dangerous. The science is clear: CBD can change how your body handles drugs - sometimes with life-threatening results.
There’s no reason to avoid CBD if you’re healthy and off meds. But if you’re on anything that keeps you alive - blood thinners, heart meds, transplant drugs, seizure control - you need to treat CBD like a drug. Because it is.
Ask your doctor. Talk to your pharmacist. Get blood tests if needed. Don’t risk your health because a bottle says "all-natural."
Can I take CBD with my blood thinner like warfarin?
No - not without close medical supervision. CBD can make warfarin much stronger, increasing your risk of dangerous bleeding. Seven documented cases showed patients needed major dose adjustments after starting CBD, and two had serious complications. If you’re on warfarin, avoid CBD unless your doctor orders regular INR blood tests and adjusts your dose accordingly.
Does CBD interact with antidepressants or anxiety meds?
Yes, especially with SSRIs like sertraline or benzodiazepines like Xanax. CBD can raise blood levels of these drugs, increasing side effects like dizziness, drowsiness, and impaired coordination. It can also worsen sedation, making falls or accidents more likely. If you’re on these meds, talk to your doctor before using CBD - and never combine them without monitoring.
Is CBD safe if I only use it once in a while?
Not necessarily. CBD’s enzyme-blocking effect can last for days, even after you stop taking it. A single dose might not cause immediate problems, but if you’re on a drug with a narrow therapeutic index - like warfarin or seizure meds - even a short-term spike in blood levels can be dangerous. Consistent use increases risk, but occasional use doesn’t eliminate it.
Can I use CBD if I have liver problems?
No. CBD is contraindicated in people with moderate to severe liver impairment. Clinical trials of Epidiolex showed elevated liver enzymes in 20% of users - a sign of liver stress. If you already have fatty liver disease, hepatitis, or cirrhosis, CBD could worsen your condition. Always get your liver function tested before using CBD, especially if you’re on other medications that affect the liver.
Are CBD gummies or oils riskier than topicals?
Oral forms - gummies, oils, capsules - are far riskier because they enter your bloodstream and affect your liver enzymes. Topicals like creams or patches are less likely to cause interactions since they’re absorbed through the skin and rarely reach systemic levels. But if you apply them to large areas, broken skin, or use them daily, some CBD may still get into your blood. For safety, assume oral CBD is the main concern.
Should I stop my meds if I want to try CBD?
Never stop prescribed medication without your doctor’s guidance. Stopping blood thinners, seizure meds, or heart drugs suddenly can be deadly. If you want to try CBD, work with your doctor to assess the risk, monitor your blood levels, and adjust doses safely - if at all. CBD should never replace a prescribed treatment unless under strict medical supervision.

David Cunningham
Been using CBD for back pain for a year now, never touched my blood pressure med. Just spaced them out and kept an eye on how I felt. No issues. But yeah, if you’re on warfarin or seizure stuff, don’t be dumb.
Rahul Kanakarajan
Of course it’s dangerous. You people think ‘natural’ means ‘safe’ like it’s some kind of yoga retreat. CBD is a drug. It’s not herbal tea. Stop treating your liver like a buffet.
Ravi Kumar Gupta
Bro in India we’ve been using ayurvedic oils with turmeric and ashwagandha for centuries with meds and never had a problem. Why is this any different? Maybe your doctors just don’t understand real medicine.
Holly Schumacher
Actually, the CYP3A4 inhibition is dose-dependent and nonlinear, and the 2023 J Clin Pharmacol paper you cited explicitly states that even sub-10mg doses show measurable enzyme suppression in vitro - and that’s without considering genetic polymorphisms in CYP2C19. So no, there’s no safe threshold. You’re not just ‘being cautious,’ you’re potentially poisoning yourself if you’re on a narrow-therapeutic-index drug. I’ve seen three ER cases from this exact combo. This isn’t opinion. It’s pharmacokinetics.
Jessica Correa
I get what you’re saying but I’ve been on sertraline for 8 years and started 15mg CBD oil for anxiety last month and I’m fine. No dizziness, no weird fatigue. Maybe it’s different for everyone? I just listen to my body and if something feels off I stop
james lucas
im so glad someone finally said this. i was on lipitor and started taking cbd gummies for sleep and i swear i felt like my legs were made of wet cement. went to the doc and my liver enzymes were through the roof. they said it was probably the cbd. i stopped it and 2 weeks later i felt like a new person. why dont more people talk about this? its not just about warfarin. its everything. i thought cbd was just chill stuff but nah. its a silent ninja in your liver
luke young
Thanks for laying this out so clearly. I’m on levothyroxine and was thinking about trying CBD for stress. Now I’m not. I’ll talk to my pharmacist tomorrow. You’re right - just because it’s plant-based doesn’t mean it’s harmless. I appreciate the practical steps.
Nikhil Chaurasia
I respect your concern, but I’ve seen too many people panic over supplements. My uncle takes warfarin and CBD daily - his INR is stable, his doctor monitors it, and he’s sleeping better than ever. The issue isn’t CBD. It’s people avoiding doctors and self-medicating without oversight. This isn’t a warning - it’s a call to engage with your care team.
manish chaturvedi
As a medical educator in Delhi, I have seen patients on antiepileptics self-medicate with CBD due to misinformation on social media. The consequences are severe: tremors, confusion, hospitalizations. Education, not fear, is the solution. Please consult your physician. Do not rely on Reddit or influencers. Your life depends on accurate information.
New Yorkers
It’s not about CBD being evil. It’s about how we’ve turned healing into a consumer sport. We want quick fixes, natural vibes, and no doctor visits. But biology doesn’t care about your aesthetic. It’s chemistry. And chemistry doesn’t do vibes. It does math. And the math says: stop treating your liver like a TikTok trend.