Chronic pain doesn’t just hurt. It wears you down-sleepless nights, canceled plans, the constant fear that the next flare-up will steal another day. You’ve tried meds, physical therapy, even injections. But the pain sticks. And if you’re like most people, you’re tired of treatments that only mask the problem instead of changing how you live with it. That’s where CBT for chronic pain comes in. Not as a cure, but as a real, practical way to take back control.
What CBT for Chronic Pain Actually Does
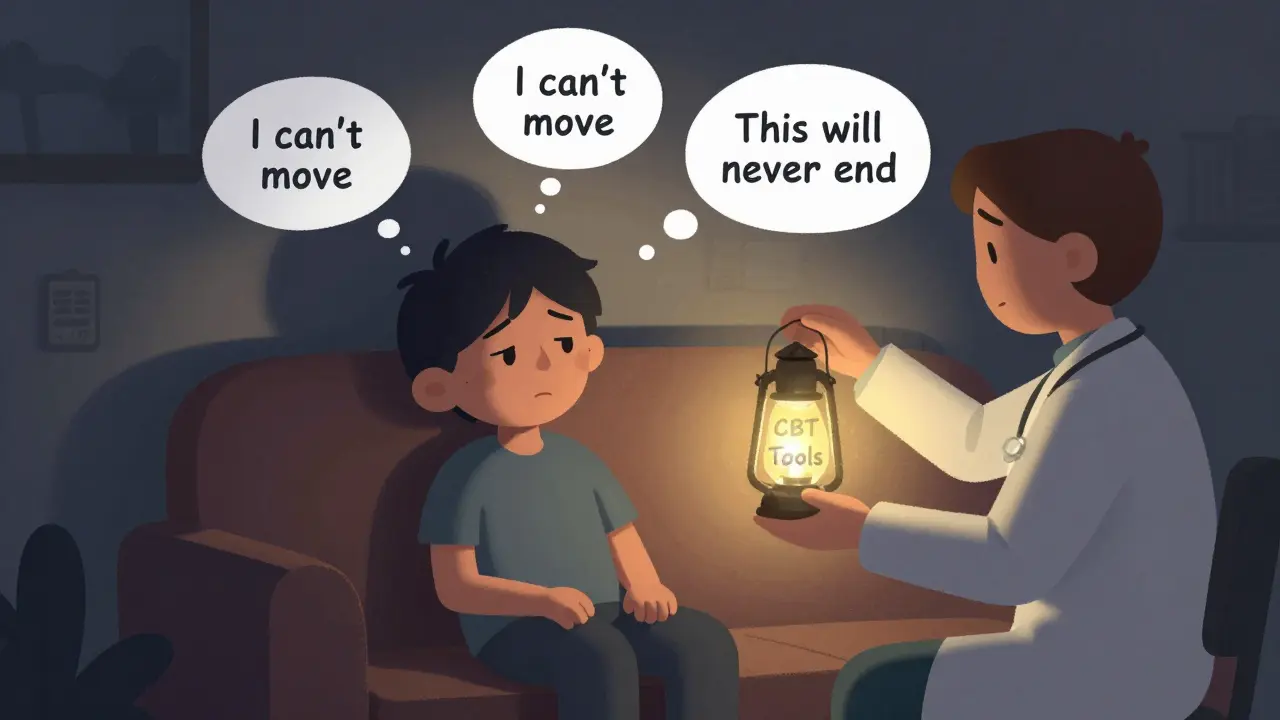
Cognitive Behavioral Therapy for chronic pain isn’t about pretending the pain isn’t there. It’s not magic. It doesn’t erase nerve damage or fix a herniated disc. What it does is change how your brain reacts to pain. When pain lasts longer than three months, your nervous system gets stuck in overdrive. Your mind starts linking movement with danger. You avoid walking, lifting, even laughing-because your brain thinks it’ll make things worse. That’s when pain turns into a cycle: fear → avoidance → weakness → more pain.
CBT breaks that cycle. It teaches you to spot the thoughts that make pain feel worse-like “I’ll never get better” or “If I move, I’ll tear something.” Then it gives you tools to replace them. Instead of thinking “I can’t do anything,” you learn: “I can do less today, and that’s okay.” It’s not about positive thinking. It’s about realistic thinking.
How It Works: The Core Tools
A typical CBT program for pain runs 8 to 12 weeks, with weekly 60- to 90-minute sessions. You don’t need to be a therapist to use these techniques-they’re designed to be practical.
- Pain neuroscience education: You learn how pain works in the body-not just as damage, but as an output of your nervous system. This alone reduces fear. When you understand that pain ≠ tissue damage, you stop avoiding movement out of terror.
- Activity pacing: Instead of going all-out on good days and crashing for days after, you learn to spread activity evenly. Walk 10 minutes twice a day instead of 20 once. It sounds simple, but it stops the boom-bust cycle that keeps pain flaring.
- Cognitive restructuring: You write down thoughts like “I’m a burden” or “This pain controls my life.” Then you challenge them with evidence: “I helped my neighbor with groceries last week,” or “I still cook dinner every night.”
- Relaxation training: Deep breathing, progressive muscle relaxation, mindfulness. These don’t eliminate pain, but they lower your body’s stress response-which directly lowers pain sensitivity.
- Behavioral activation: You rebuild activities you’ve given up-not because the pain is gone, but because you’re learning to live with it differently. Maybe it’s gardening again, or playing with your grandkids.
These aren’t theoretical. The U.S. Department of Veterans Affairs has used this exact protocol since 2010. Their data shows 73% of participants report meaningful improvement in daily function-not because their pain disappeared, but because they stopped letting it dictate their lives.
What the Research Says
A 2023 review of 13 studies involving over 1,600 people found CBT for chronic pain consistently improved depression, anxiety, and quality of life. Pain intensity? That’s trickier. Only about 25% of studies showed significant drops in pain numbers. But here’s the key: even when pain didn’t drop, people felt better. They slept more. They moved more. They took fewer opioids.
The 2024 STAMP trial compared CBT to mindfulness therapy in 254 people with chronic low back pain on opioids. Both worked equally well. But CBT had one clear edge: 36% of participants cut their daily opioid use, compared to just 17% in the usual care group. That’s not minor. It’s life-changing.
And it’s not just for back pain. CBT helps with fibromyalgia, arthritis, neuropathic pain-even complex regional pain syndrome. It works best when pain is tied to stress, anxiety, or depression-which is true for most long-term pain sufferers.

Who It Works For (And Who It Doesn’t)
CBT isn’t a one-size-fits-all fix. It shines when:
- You’re stuck in fear-avoidance (you skip activities because you’re scared of pain)
- You’re dealing with depression or anxiety alongside your pain
- You’re trying to reduce or stop opioids
- You’re motivated to learn new skills
It’s less effective if:
- Your pain is purely neuropathic (like diabetic nerve pain) with no emotional component
- You’re in severe, constant pain and can’t focus on exercises
- You don’t believe psychological tools can help physical pain (this is common-more on that below)
One 2023 study even found no benefit for men in some cases. That’s why experts now say CBT should be personalized. If you’re a 65-year-old woman with osteoarthritis and insomnia, your CBT plan will look different than a 35-year-old man with post-surgical pain and PTSD.
How It Compares to Other Options
Let’s say you’re choosing between CBT, physical therapy, and medication.
| Treatment | Best For | Pain Reduction | Function Improvement | Risk of Side Effects |
|---|---|---|---|---|
| CBT for chronic pain | Emotional impact, fear, opioid use, depression | Moderate (25% of studies show improvement) | Strong (73% report meaningful gains) | None |
| Physical therapy | Muscle strength, mobility, joint function | Moderate | Strong | Low (risk of flare-ups) |
| Opioids | Acute flare-ups | High (short-term) | Weak | High (addiction, tolerance, overdose) |
| Mindfulness therapy | Stress, emotional regulation | Moderate | Strong | None |
Here’s the truth: CBT alone won’t fix a torn ligament. But it can help you move without fear. And when you combine CBT with physical therapy, studies show 40% greater improvement in function than CBT alone. That’s why top pain clinics now use multidisciplinary teams-physiotherapists, psychologists, doctors-all working together.
Real People, Real Results
Reddit threads from r/ChronicPain show thousands of people sharing their CBT experiences. One woman wrote: “I used to cancel plans every weekend. After 10 sessions, I went to my niece’s wedding. I sat in a chair, didn’t dance, but I was there. That meant more than any pill ever did.”
Another man, 52, with failed back surgery syndrome: “I thought CBT was just talking. Turns out, I was the one keeping myself stuck. Learning to pace my walks? That changed everything. I’m not pain-free. But I’m alive again.”
But it’s not all success stories. Some people say: “It didn’t fix my pain.” Or “I got frustrated when the therapist said ‘change your thoughts.’” That’s valid. CBT isn’t about denying reality. It’s about changing your relationship with it. If your therapist pushes you to “think positive,” find someone else. Good CBT is collaborative, not preachy.
Getting Started
First, talk to your doctor. Ask if they can refer you to a psychologist trained in CBT for chronic pain. Look for credentials: licensed clinical psychologist with training in pain psychology. The VA’s protocol is the gold standard-many private therapists follow it.
If you can’t find a local therapist, digital CBT apps are now FDA-cleared and backed by research. Programs like MyPainCoach or PainCourse offer structured lessons you can do at home. A 2021 study found video-based CBT was just as effective as in-person.
Insurance coverage? It’s messy. Medicare covers only 10 sessions a year. Commercial insurers vary: UnitedHealthcare covers 12, Aetna covers 8. You might need to appeal. But if you’re reducing opioids or improving function, it’s worth pushing for.
What to Expect in Your First Session
You’ll fill out questionnaires: the Pain Catastrophizing Scale, the Brief Pain Inventory. You’ll talk about your pain history, what you’ve tried, what made it worse. The therapist won’t fix your back. They’ll ask: “What do you believe happens when you move?” “What’s the worst thing you think could happen?” “What’s one thing you’d do if pain wasn’t holding you back?”
Then you’ll get homework. Not busywork. Real tasks: “Walk 5 minutes today. Write down what you thought before, during, and after.” “Write down one thought about your pain that made you feel helpless. Now write a more balanced version.”
It’s not easy. Some days, you’ll want to quit. But the people who stick with it-especially those who complete at least 8 sessions-are the ones who see results.
Why This Matters Now
The opioid crisis didn’t happen because people were weak. It happened because we had no better tools. CBT for chronic pain isn’t a luxury. It’s a necessity. With over 80% of chronic pain patients dissatisfied with current treatments, we need options that don’t come with addiction risks.
And the future is getting better. The NIH is investing $14.2 million to make CBT more personalized. Wearables are being tested to track activity levels and give real-time feedback. Brief 4- to 6-session versions are showing promise for people who can’t commit to 12 weeks.
Chronic pain is exhausting. But you don’t have to let it define you. CBT doesn’t promise a pain-free life. It promises a life where pain doesn’t run the show.
Is CBT for chronic pain just in my head?
No. Chronic pain is real-it’s happening in your nervous system. CBT doesn’t say the pain is imaginary. It says your brain has learned to amplify it. CBT helps retrain how your brain responds to pain signals, which changes how much you suffer. It’s not about thinking happy thoughts. It’s about breaking the cycle of fear and avoidance that keeps pain stuck.
How long until I see results from CBT for chronic pain?
Most people start noticing changes in 4 to 6 weeks-like sleeping better, moving more, or feeling less anxious about pain. But real improvement in daily function usually takes 8 to 12 weeks. The key is consistency. People who complete at least 8 sessions are 2.3 times more likely to see lasting results than those who drop out early.
Can CBT help me stop taking opioids?
Yes. In the 2024 STAMP trial, 36% of people using CBT reduced their daily opioid use, compared to only 17% in the usual care group. CBT doesn’t eliminate pain, but it reduces the fear and distress that make people rely on opioids. It gives you tools to manage flare-ups without medication. Always work with your doctor to taper safely.
Do I need a therapist, or can I do CBT on my own?
You can start with digital programs like MyPainCoach or PainCourse-both are FDA-cleared and backed by research. But working with a trained therapist increases success rates. Therapists help you spot blind spots, adjust techniques, and stay motivated. If you’re struggling with depression, anxiety, or trauma, a therapist is essential.
Is CBT covered by insurance?
It depends. Medicare covers only 10 sessions per year. Private insurers vary: UnitedHealthcare covers 12, Aetna covers 8. Many plans require pre-authorization. Ask your provider if they cover “Cognitive Behavioral Therapy for Chronic Pain” specifically. If denied, appeal using the evidence: CBT reduces opioid use and improves function, which lowers long-term healthcare costs.
What if CBT doesn’t work for me?
It’s not a failure. CBT works best when combined with other treatments. If you’ve tried it and didn’t improve, consider adding physical therapy, acupuncture, or a pain management clinic. Some people need more time, or a different therapist. Others benefit from mindfulness or acceptance and commitment therapy (ACT). The goal isn’t to find the one magic solution-it’s to find what helps you live better.
If you’re tired of pain controlling your life, CBT gives you back your power-not by making the pain vanish, but by changing how you respond to it. That’s not just therapy. That’s freedom.

Sachin Bhorde
CBT for chronic pain is legit. I’ve been through it for my fibro, and the pain neuroscience ed was a game-changer. Turns out, my brain was screaming ‘DANGER!’ every time I stood up-even when there was zero tissue damage. Learning that pain ≠ harm? That’s the first step. Activity pacing? Yeah, I used to do 10k steps on good days and crash for 3 days. Now I do 2k twice a day. It’s boring, but it works. No magic, just neuroplasticity.
Joe Bartlett
Looks like another American therapy fad. We’ve got NHS pain clinics here in the UK that actually treat the body, not just the mind. CBT won’t fix a degenerated disc. Go lift weights, get a physio, stop overthinking.
Salome Perez
As someone who’s worked with chronic pain patients across 12 countries, I’ve seen CBT transform lives-not because it ‘fixes’ pain, but because it restores agency. In rural India, a woman with arthritis learned to weave again by pacing her movements. In rural Tennessee, a veteran stopped opioid use after realizing his fear of movement was worse than the pain. This isn’t ‘just in your head.’ It’s your head learning to stop sabotaging your body. And yes, it’s messy, human, and deeply brave.
Kent Peterson
Wait-so you’re telling me that after spending $20,000 on MRIs, epidurals, and nerve blocks, the solution is… talking? And you cite a 2024 STAMP trial? That’s one study. One! And you ignore the 2022 meta-analysis in JAMA Neurology that showed CBT had no significant effect on pain thresholds in neuropathic populations? And you say it’s ‘evidence-based’? Where’s the double-blind RCT? Where’s the placebo control? This reads like a pharmaceutical industry ad for non-pharmaceutical alternatives. I’m not buying it.
Josh Potter
YESSSS. I was on 80mg oxycodone a day. CBT didn’t make the pain disappear-but it made me stop being a prisoner in my own body. I started walking my dog again. I held my daughter’s hand at her graduation. I cried. Not from pain. From freedom. If you think this is ‘just mindset,’ you’ve never lived with it. Do the work. It’s hard. But it’s worth it.
Evelyn Vélez Mejía
The epistemological shift here is profound: pain as a neuropsychological phenomenon rather than a purely somatic one. This reframing dismantles the Cartesian dualism that has dominated pain medicine for centuries. The nervous system does not merely transmit signals-it constructs experience. CBT, therefore, is not a palliative, but a phenomenological recalibration. The data supports this: improved function without reduced nociception indicates a reorganization of the salience network. This is not therapy. It is neurophenomenological liberation.
Anna Giakoumakatou
Oh, wonderful. Another opiate-free utopia where people are told to ‘think differently’ while their spine collapses. How noble. I’m sure the insurance companies love this-cheaper than surgery, and you can blame the patient if it ‘doesn’t work.’ Tell me, does the therapist also recommend positive affirmations while you’re lying on the floor, unable to stand? How poetic.
Sam Clark
Thank you for this comprehensive, compassionate overview. I’ve worked as a pain management coordinator for over a decade, and I’ve seen firsthand how CBT, when delivered with fidelity and empathy, restores dignity to those who feel broken. I’d only add: the most successful outcomes occur when CBT is integrated with physical rehabilitation-not as an alternative, but as a partner. And yes, finding the right therapist matters. Look for someone who says, ‘I’m here to walk with you,’ not ‘I’m here to fix you.’