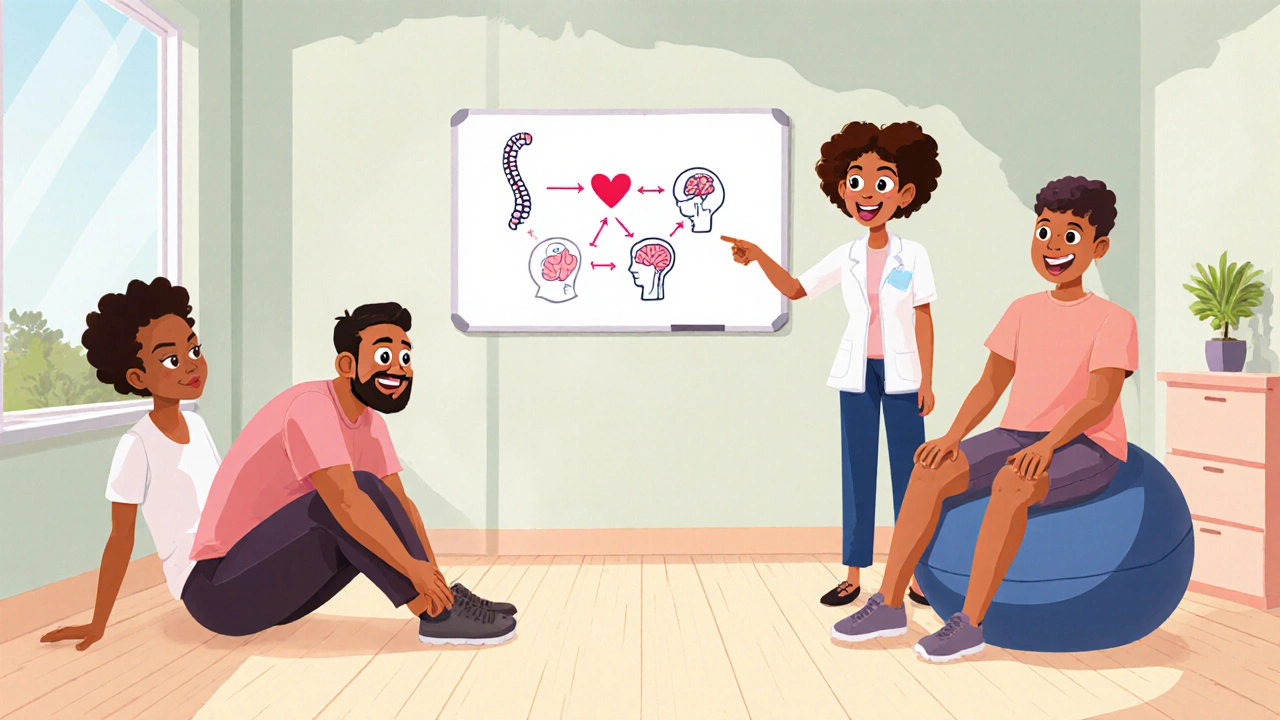
Chronic back pain isn't just a sore back that won't go away. It's pain that lasts longer than 12 weeks, even after an injury has healed. About 8% of Americans live with it, according to the National Institutes of Health. And unlike acute pain - which tells you something’s wrong - chronic pain becomes its own problem. It rewires how your nervous system works. That’s why simply popping pills or resting won’t fix it. You need a plan that targets the body, the brain, and daily habits.
Physical Therapy: The Most Effective First Step
Physical therapy isn’t just stretching and massage. It’s a science-backed program designed to retrain your body. The American College of Physicians says it should be the first treatment you try - before any medication. Why? Because it works better long-term.
Good physical therapy for chronic back pain includes five key pieces:
- Pain tolerance assessment - Your therapist doesn’t push you to the limit. They find your safe zone and build from there.
- Posture retraining - Slouching at your desk or lifting wrong changes how your spine carries weight. Correcting this reduces pressure on nerves and discs.
- Core strengthening - Not crunches. Focus is on deep muscles like the transverse abdominis and multifidus. These are your body’s natural back braces.
- Flexibility and stretching - Tight hamstrings or hip flexors pull on your lower back. Stretching them improves spinal mobility by 15-25%, according to OIP’s 2024 data.
- Aerobic conditioning - Walking, swimming, or cycling increases blood flow to spinal tissues by 30-40%. More blood means less inflammation and faster healing.
Studies show 78% of people with chronic back pain see meaningful improvement with physical therapy. That’s compared to just 52% with medications alone. But here’s the catch: it only works if you do the exercises at home. Patients who stick with their home routine have an 82% success rate. Those who don’t? Only 45%.
Medications: Use Them Wisely, Not as a Crutch
Medications can help, but they’re not a cure. And the old habit of reaching for opioids? That’s over. In 2016, nearly half of chronic back pain patients got opioids. By 2024, that number dropped to 12% - thanks to the opioid crisis and updated CDC guidelines.
Today, doctors follow a tiered approach:
- First-line: NSAIDs - Ibuprofen (400mg three times daily) or naproxen (500mg twice daily). They reduce inflammation and give 30-40% pain relief for 65% of users. But they’re not harmless. Up to 20% of long-term users get stomach ulcers or kidney issues.
- Second-line: Muscle relaxants and nerve agents - Cyclobenzaprine helps with spasms. Gabapentin (starting at 100mg nightly, slowly increased) targets nerve pain. But gabapentin causes dizziness and brain fog in many. One Reddit user switched from 900mg daily to duloxetine because “I couldn’t function.”
- Third-line: SNRIs - Duloxetine (60mg daily) is the most studied for chronic back pain. In a 2022 NIH review of nearly 10,000 patients, it helped 67% of people, with 50% pain reduction. But 25% get nausea, 15% feel dizzy.
Here’s the reality: no single pill works for everyone. Dr. Richard Wagner from University of Utah Health says, “Sometimes that comes down to a combination of medications.” But even then, side effects often outweigh benefits. That’s why medications are best used short-term while you build strength and movement through therapy.
Self-Management: The Secret Weapon
You can’t spend every day in a therapist’s office. That’s why self-management is the most powerful tool you have. It’s not about willpower. It’s about structure.
Programs like UCSF’s Chronic Pain Toolkit teach you how to:
- Track your pain daily (what triggers it, what eases it)
- Set realistic movement goals (e.g., “walk 10 minutes, twice a day”)
- Use pacing - not pushing through pain, but working in short bursts with rest
- Manage stress with breathing or mindfulness (stress tightens muscles and worsens pain)
Harvard Health found that people who stick with self-management for 8-12 weeks see 40-50% pain reduction. But only 63% actually stick with it. Why? Because it’s hard. It takes 20-30 minutes a day. And many don’t feel immediate results.
But those who do? They’re the ones who get their lives back. On Reddit, user “BackPainWarrior87” said: “Six months of physical therapy brought my pain from 8/10 to 3/10. The exercises are brutal to maintain - but worth it.”
What Doesn’t Work - And Why
Not all treatments are equal. Some sound good but don’t deliver.
- Bed rest - Staying in bed for days makes muscles weaker and pain worse.
- Long-term opioids - Not only addictive, they can cause opioid-induced hyperalgesia - meaning your body becomes more sensitive to pain over time.
- Spinal injections for everyone - Epidural steroid shots help 60-70% of people with nerve root pain, but only if it’s the right kind of pain. For mechanical back pain? Often useless.
- “Miracle” devices - TENS units, magnetic braces, or laser therapy? No strong evidence they change long-term outcomes.
Also, don’t expect perfection. Even the best treatments rarely erase pain completely. The goal isn’t “no pain.” It’s “enough pain relief to move, work, and live.”
Who Gets the Best Results?
Success isn’t random. It’s tied to who you are and how you approach treatment.
- Age - People 35-54 use physical therapy most. Those 55-74 rely more on meds. Why? Older adults often have more conditions (like arthritis) that meds help manage.
- Insurance - Medicare only covers 20 physical therapy visits a year unless you get special approval. Many drop out after hitting that limit. Private insurers vary widely.
- Work status - Only 38% of working adults can keep up with therapy schedules. That’s why home exercises are non-negotiable.
- Pain type - Physical therapy shines for mechanical pain (movement-related). Medications work better for inflammatory conditions like ankylosing spondylitis. For complex nerve pain? You need a team - PT, meds, counseling.

What’s Changing in 2025
The field is moving fast. The NIH launched a $45 million precision medicine study in early 2024 to figure out which patients respond best to which treatments. Are you someone who improves with movement? With gabapentin? With mindfulness? The goal is to match you to the right combo - not guess.
Also, new non-opioid drugs are coming. HTX-011 (a dual-acting local anesthetic) and AXS-07 (a fast-acting NSAID) are already fast-tracked by the FDA. And clinics are adopting “stepped-care” models: start with PT and self-management, add meds if needed, then consider injections or stimulators only if everything else fails.
The bottom line? The future isn’t one magic fix. It’s a personalized mix - and you’re the one who has to stick with it.
Real Talk: What to Do Right Now
If you’re stuck with chronic back pain, here’s your action plan:
- See a physical therapist - Ask your doctor for a referral. Don’t wait. Start moving, even if it’s slow.
- Stop relying on OTC painkillers - If you’re taking ibuprofen daily for more than 3 months, talk to your doctor. The risks add up.
- Start a pain journal - Note what you did, how you felt, and what helped. Patterns emerge.
- Do 10 minutes of movement every day - Walk, stretch, or do a simple core routine. Consistency beats intensity.
- Find community - Join PainConnection.org or the r/ChronicPain subreddit. You’re not alone.
Chronic back pain doesn’t vanish overnight. But with the right approach, it can stop controlling your life. The tools are here. You just have to use them - one day at a time.
Can physical therapy cure chronic back pain?
Physical therapy doesn’t always “cure” chronic back pain, but it’s the most effective way to reduce it long-term. Studies show 78% of patients achieve meaningful improvement - meaning less pain, better movement, and more daily function. The key is consistency: patients who do their home exercises have an 82% success rate.
Are opioids still used for chronic back pain?
Opioids are rarely used today for chronic back pain. In 2024, only 12% of patients received them - down from 45% in 2016. CDC guidelines now recommend them only as a last resort, after all other options fail. Long-term use can worsen pain through opioid-induced hyperalgesia and carries high risks of dependence and overdose.
What’s the best medication for chronic back pain?
There’s no single “best” medication. NSAIDs like ibuprofen help with inflammation but risk stomach and kidney issues. Gabapentin works for nerve pain but causes brain fog. Duloxetine (an SNRI) helps 67% of patients with moderate pain reduction, but causes nausea in 25%. Most people need a combination, tailored by their doctor.
How long does physical therapy take to work for back pain?
Most people start feeling better after 4-6 weeks of consistent therapy, with weekly sessions and daily home exercises. Full improvement often takes 8-12 weeks. The goal isn’t quick relief - it’s rebuilding strength and movement patterns so pain doesn’t return.
Can I manage chronic back pain without medication?
Yes - many people do. Physical therapy, daily movement, stress management, and pacing techniques can reduce pain by 40-50% without any drugs. But for some, especially those with nerve-related pain or inflammation, a low-dose medication like duloxetine or gabapentin adds important support. The best results come from combining approaches.
Why do some people’s back pain never get better?
Pain that doesn’t improve usually means the treatment isn’t matched to the cause. Mechanical pain responds to movement and strength. Nerve pain needs meds like gabapentin. Inflammatory pain needs different drugs. Also, insurance limits, lack of home exercise, or mental health factors like depression can block progress. A multidisciplinary approach - PT, meds, counseling - often works where single treatments fail.

Kihya Beitz
Oh wow, another ‘just do PT and you’ll be fine’ pamphlet. Let me guess - you’ve never had a disc that’s literally screaming when you sit down? I’ve done PT. I’ve done the core stuff. I’ve done the walking. My back still feels like it’s being slowly crushed by a Volkswagen. And no, I don’t have ‘bad habits’ - I have a spine that betrayed me. Thanks for the lecture, though.
Jennifer Walton
Pain is not a problem to be solved. It is a signal that the body has become a landscape of unspoken grief. We treat it like a machine glitch. But the spine remembers what the mind forgets.
Jessica Chambers
78% improvement with PT? That’s nice. 😅 But what about the 22% who are just… stuck? And who’s paying for 12 weeks of therapy when your insurance cuts you off at 20 visits? 🤷♀️
Shyamal Spadoni
They say PT works but they never tell you the real reason - the pharmaceutical industry hates it. Why? Because if people just walked and stretched, they wouldn’t need your 800-dollar-a-month gabapentin prescriptions. The CDC? CIA front. NSAIDs? Made by Big Pharma to keep you hooked on stomach bleeding. I’ve seen the docs - they’re all on the payroll. I’ve been doing isometric breathing and cold showers for 3 years now. My pain’s gone. No pills. No PT. Just truth.
Ogonna Igbo
You Americans think your way is the only way. In Nigeria we don’t waste time on PT. We pray. We use herbs. We dance. We lift heavy things. We don’t sit around counting reps like you’re in some gym cult. Your back pain is weakness. We have real pain - we carry water on our heads, walk 10km to clinic, and still smile. You need discipline not a checklist.
BABA SABKA
Let’s be real - this whole ‘stepped-care’ model is just corporate medicine’s way of delaying the inevitable. You want to know what actually works? Movement. Not the fancy-ass ‘core strengthening’ nonsense. Just move. Walk. Squat. Carry. Bend. Your spine evolved to do this. You turned your body into a desk statue and now you’re surprised it’s broken. Stop overcomplicating it. Your therapist isn’t your therapist - they’re your accountability coach. And yes, you’re lazy. But you can change.
Chris Bryan
They’re hiding the truth. Chronic pain isn’t about muscles or nerves - it’s about the government’s glyphosate-laced food supply poisoning our nervous systems. You think PT helps? Try eating organic, avoiding fluoride, and sleeping in a Faraday cage. I’ve been pain-free for 14 months since I stopped using municipal water. The CDC doesn’t want you to know this. They’re paid by Bayer.
Jonathan Dobey
Ah yes - the sacred liturgy of modern pain management: PT, NSAIDs, duloxetine, journaling, and the obligatory Reddit testimonial from ‘BackPainWarrior87’ as if he’s some ascetic monk who tamed the dragon of inflammation. How quaint. The real tragedy isn’t the pain - it’s the pathetic, performative optimism that surrounds it. We’ve turned suffering into a productivity hack. ‘Do 10 minutes a day!’ Like your spine is a garden you can prune into submission. Pain is not a bug to be patched. It’s the echo of your soul screaming in a world that commodifies even your agony. You don’t need a toolkit. You need to stop pretending you’re in control.
ASHISH TURAN
Just want to say - I’ve been doing this for 5 years. PT didn’t fix me overnight. But doing the exercises every morning, even when I didn’t want to, changed everything. I still have pain. But now I don’t let it decide my day. No magic. Just consistency. And yeah, the journal helps. I track everything - sleep, stress, what I ate, how I moved. Turns out, pizza and sitting for 8 hours don’t mix well with lumbar discs. You’re not broken. You’re just out of rhythm. Find yours.