QT Prolongation Risk Calculator
QT Prolongation Risk Assessment
When doctors prescribe antidepressants, they don’t just look at mood improvement. They also check for hidden risks-like changes in heart rhythm. Two commonly used SSRIs, citalopram and escitalopram, carry a quiet but serious danger: QT prolongation. This isn’t just a footnote in the prescribing info. It’s a real, measurable risk that changed how these drugs are used today.
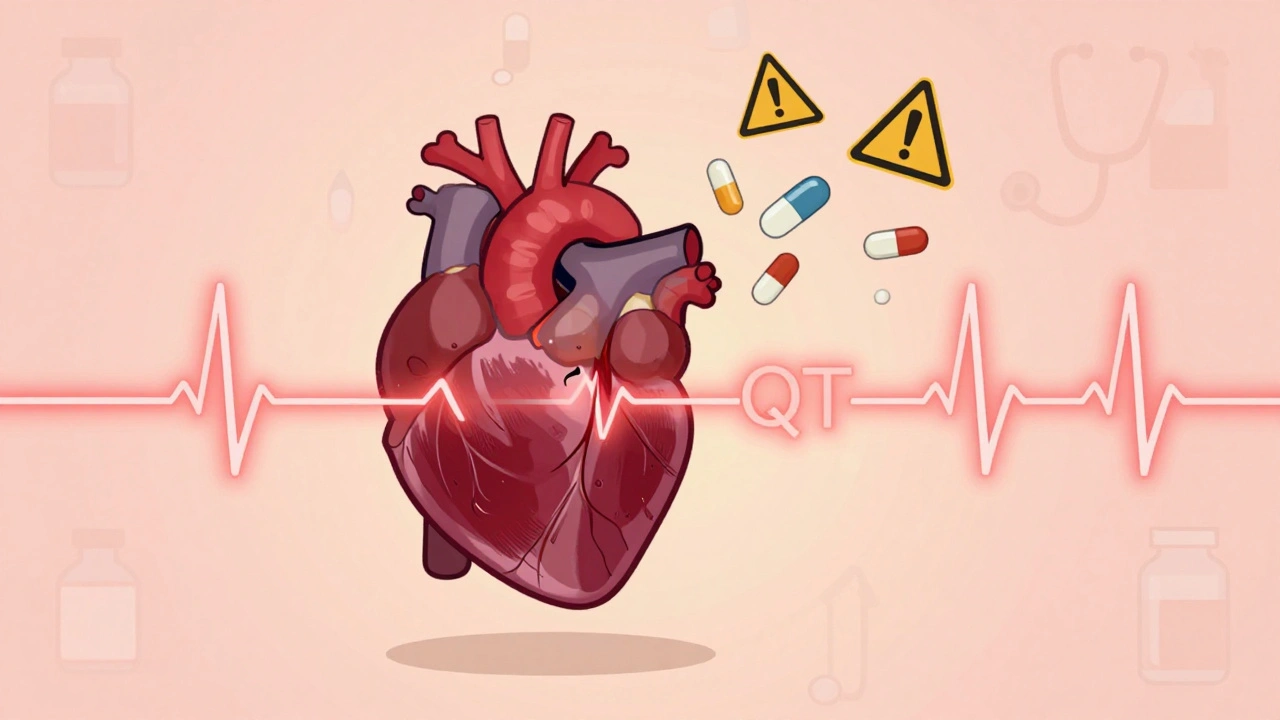
What QT Prolongation Actually Means
Your heart beats because of electrical signals. The QT interval on an ECG measures how long it takes the heart’s lower chambers to recharge between beats. If that interval gets too long, your heart can slip into a dangerous rhythm called Torsade de Pointes. It’s rare, but it can lead to sudden cardiac arrest.
Both citalopram and escitalopram block a specific potassium channel (hERG) in heart cells. That slows down the heart’s recharge time. It’s not unique to these drugs-some antibiotics, antifungals, and older antidepressants do the same thing. But with SSRIs, this risk became a major focus after 2011.
The 2011 Safety Shift
Before 2011, citalopram was often prescribed at 60 mg daily. That changed overnight. The FDA, MHRA, and other global agencies reviewed data showing clear, dose-dependent QT prolongation. The numbers didn’t lie:
- At 20 mg, citalopram extended QTc by about 8.5 milliseconds
- At 40 mg, that jumped to 12.6 ms
- At 60 mg, it soared to 18.5 ms
Escitalopram, the purified S-enantiomer of citalopram, showed less effect:
- 10 mg: +4.5 ms
- 20 mg: +6.6 ms
- 30 mg: +10.7 ms
These aren’t random spikes. A QTc interval over 500 ms-or a change of 60 ms from baseline-is considered clinically dangerous. The FDA flagged citalopram specifically, but the UK’s MHRA warned about both drugs. That’s why dose limits were slashed.
Current Dose Limits You Can’t Ignore
Today, you won’t see a prescription for 60 mg of citalopram. Regulatory agencies set hard caps:
- Citalopram: Max 40 mg/day for adults under 65; max 20 mg/day for those 65 and older
- Escitalopram: Max 20 mg/day for adults; max 10 mg/day for patients over 65
Why the difference for older adults? Their livers process these drugs slower. Higher blood levels = higher risk. Even a 10 mg dose of escitalopram can be too much for someone in their 70s with kidney or liver issues.
These aren’t suggestions. They’re safety rules. Prescribing above these limits now carries legal and clinical liability.
Who’s at Highest Risk?
Not everyone on these drugs will have a problem. But some people are walking into danger without knowing it:
- People with existing long QT syndrome (congenital or acquired)
- Those with bradycardia (slow heart rate)
- Patients recovering from a heart attack
- Anyone taking other QT-prolonging drugs-like certain antibiotics, antifungals, or antiarrhythmics
- People with low potassium or magnesium levels
Electrolyte imbalances are easy to miss. A patient on diuretics for high blood pressure? That’s a red flag. A senior with poor diet or vomiting from the flu? That’s a hidden risk. Always check electrolytes before starting or increasing the dose.

Citalopram vs. Escitalopram: Which Is Safer?
Escitalopram is often chosen over citalopram-not because it’s risk-free, but because it’s less risky. The same 2013 analysis found that while both drugs show similar patterns of QT prolongation, citalopram’s effect is stronger at every dose. At 40 mg, citalopram adds nearly twice the QTc prolongation as escitalopram at 20 mg.
That’s why many clinicians now default to escitalopram, especially for patients with heart disease, older adults, or those on multiple medications. The cost is higher, but the safety margin is wider.
Still, escitalopram isn’t harmless. At 30 mg, it still pushes QTc past 10 ms. That’s why the max dose stays at 20 mg for most adults.
Other Antidepressants and QT Risk
Not all SSRIs are equal. Fluoxetine, sertraline, and paroxetine have minimal QT effects. They’re often safer picks for patients with cardiac history.
SNRIs like venlafaxine carry low risk at normal doses, but overdose can be dangerous. Tricyclic antidepressants (TCAs) like amitriptyline are worse than citalopram-QT prolongation is common and well-documented. They’re rarely first-line anymore, especially in older patients.
If someone’s had a bad reaction to citalopram, switching to sertraline or fluoxetine is often the smart move. No need to gamble with another SSRI that carries the same heart risk.
Monitoring: What You Actually Need to Do
You don’t need an ECG for every patient. But you do need to know who needs one:
- Get a baseline ECG before starting citalopram or escitalopram if the patient is over 65, has heart disease, or takes other QT-prolonging drugs
- Repeat the ECG after 2-4 weeks if you increase the dose
- Check electrolytes if the patient is on diuretics, has diabetes, or has had recent illness
- Don’t start these drugs in patients with QTc over 450 ms (men) or 470 ms (women)
Many primary care doctors skip the ECG because they think the risk is too low. But when a rare event happens, it’s not low anymore. One patient’s sudden cardiac arrest isn’t a statistical anomaly-it’s a preventable tragedy.
Why These Limits Still Work
Some argue that a 10-20 ms QTc increase isn’t clinically significant. That’s true for most healthy people. But medicine isn’t about averages. It’s about protecting the vulnerable.
Studies since 2011 show that when these dose limits are followed, the rate of serious arrhythmias stays extremely low. The risk isn’t gone-but it’s managed. That’s the goal.
These drugs still help millions. They’re effective, well-tolerated, and often life-changing. But their power comes with responsibility. Prescribing them now means knowing the numbers, checking the heart, and never assuming a patient is too young or too healthy to be at risk.
What to Do If You’re Already on a High Dose
If you’ve been on 40 mg of citalopram for years without issues, don’t panic. But do talk to your doctor. There’s no benefit to staying at the upper limit if you’re stable. Lowering the dose-even to 20 mg-can reduce long-term cardiac strain without hurting antidepressant effect.
Escitalopram at 10 mg often works just as well as citalopram at 40 mg. Many patients don’t even notice the difference. The goal isn’t to use the highest possible dose. It’s to use the lowest effective dose.
Can citalopram or escitalopram cause sudden death?
Yes, but it’s rare. The main danger is Torsade de Pointes, a type of dangerous heart rhythm that can lead to cardiac arrest. This risk increases with higher doses, especially above 40 mg for citalopram or 20 mg for escitalopram. It’s most likely in people with existing heart conditions, electrolyte imbalances, or those taking other QT-prolonging drugs. Following current dose limits and avoiding high-risk combinations reduces this risk to very low levels.
Is escitalopram always safer than citalopram?
In terms of QT prolongation, yes-escitalopram has a more favorable profile. At equivalent antidepressant doses, it causes less QT interval lengthening. For patients with heart disease, older adults, or those on multiple medications, escitalopram is usually the preferred choice. But it’s not risk-free. Doses above 20 mg still carry measurable cardiac risk, and it should never be used without considering the patient’s full medication list and medical history.
Do I need an ECG before taking these drugs?
Not always, but you should get one if you’re over 65, have heart disease, take other QT-prolonging medications, or have a history of electrolyte imbalances. A baseline ECG helps identify pre-existing QT prolongation. If your QTc is already over 450 ms (men) or 470 ms (women), these drugs are generally avoided. Repeating the ECG after a dose increase is also recommended.
Can I take citalopram or escitalopram with other antidepressants?
Combining SSRIs or mixing them with other antidepressants like SNRIs or TCAs increases the risk of serotonin syndrome and QT prolongation. It’s generally not recommended unless under close supervision by a psychiatrist. Even then, the combined cardiac risk must be carefully weighed. Most guidelines advise against polypharmacy with these drugs unless absolutely necessary.
What if I miss a dose or stop suddenly?
Stopping these drugs abruptly can cause withdrawal symptoms like dizziness, nausea, or brain zaps-but it doesn’t directly trigger QT prolongation. However, if you’ve been on a high dose and stop suddenly, your body may temporarily lose the stabilizing effect of the drug, which could affect heart rhythm in rare cases. Always taper under medical supervision, especially if you have cardiac risk factors.
Final Takeaway: Safety Is About Context
Citalopram and escitalopram aren’t dangerous drugs. They’re tools. And like any tool, their safety depends on how you use them. The 2011 warnings didn’t make them unsafe-they made us smarter about using them.
For most people, escitalopram at 10 mg or citalopram at 20 mg is perfectly safe. But push those doses higher, ignore the heart risks, or combine them with other meds without checking, and you’re playing with fire.
The best prescribing isn’t about finding the strongest dose. It’s about finding the right dose for the right person. That means checking age, heart health, other meds, and electrolytes. It means choosing escitalopram over citalopram when cardiac risk is a concern. And it means never assuming someone is too young or too healthy to be affected.
These drugs changed lives. They still do. But they don’t come with a free pass. Every prescription needs a heart check.

Dan Cole
Let’s be real-this isn’t about medicine. It’s about control. The FDA didn’t slash doses because of science; they did it because lawsuits were piling up. They’d rather see a depressed person suffer than risk a single lawsuit. QT prolongation? Sure, it’s real-but so is the suicide rate in untreated depression. We’ve turned psychiatry into a liability dance, not a healing practice.
Every time they lower a dose cap, they’re not protecting patients-they’re protecting corporations. Citalopram at 40mg works. Escitalopram at 20mg? Sometimes it’s just placebo with a higher price tag. The data’s messy, but the policy? Clean. Too clean. Like a sterile operating room with no patients in it.
I’ve seen people on 60mg for a decade with perfect ECGs. No arrhythmias. No issues. But now? They’re forced down to 20mg because some 28-year-old regulator read a paper in 2011 and decided everyone’s a ticking time bomb. That’s not medicine. That’s fear dressed in a white coat.
And don’t get me started on the ‘always check electrolytes’ mantra. You want to prevent cardiac events? Fix the food system. Stop giving people Pop-Tarts and Gatorade and tell them to eat a banana. But no-let’s just slap an ECG on every 70-year-old who takes a pill. That’s the real healthcare innovation now: bureaucracy as prevention.
We’re treating depression like it’s a grenade with a pull pin. It’s not. It’s a chronic illness. And we’re treating it like a criminal offense.
Max Manoles
I appreciate the thorough breakdown, but I think the real issue is how rarely clinicians actually follow these guidelines-even when they’re aware of them. I work in a primary care clinic, and I’ve seen 3 patients in the last month on 40mg citalopram with no baseline ECG, no electrolyte check, and no mention of cardiac history. One had a pacemaker. Another was on amiodarone. Neither provider knew the risks.
It’s not that the guidelines are too strict-it’s that they’re ignored until someone dies. And then the whole system panics, overcorrects, and creates new rules that nobody remembers by next Tuesday.
The solution isn’t more caps-it’s better education. Mandatory CME on QT risk for every prescriber of SSRIs. Not a checkbox. A real module. With case studies. With ECG tracings. With consequences for skipping it.
Also-sertraline isn’t always the ‘safe’ alternative. I had a patient on sertraline 200mg who developed torsades after a GI bug and potassium crash. Dose wasn’t the issue. Context was. The drug isn’t the villain. The lack of vigilance is.
Katie O'Connell
One must acknowledge, with the utmost gravity, that the pharmacological landscape of selective serotonin reuptake inhibitors has undergone a paradigmatic recalibration since the seminal 2011 regulatory advisories. The hERG channel blockade, while a mechanistic artifact, precipitates a clinically significant electrophysiological perturbation that cannot be dismissed as statistically insignificant when viewed through the lens of population-level risk mitigation.
Moreover, the distinction between citalopram and escitalopram is not merely pharmacokinetic-it is ontological. The enantiomeric purity of escitalopram confers a superior safety profile, not by virtue of diminished potency, but by virtue of reduced off-target binding affinity-a nuance often lost in the vulgar discourse of dosage caps.
One must also interrogate the implicit anthropocentrism of the ‘healthy patient’ assumption. The human organism is not a monolith. It is a constellation of metabolic, genetic, and environmental variables. To prescribe without accounting for age, renal function, and polypharmacy is not clinical practice-it is epistemological negligence.
Therefore, the imposition of dose ceilings is not an infringement upon therapeutic autonomy, but rather a necessary bulwark against the hubris of individualized dosing in the absence of comprehensive biomonitoring.
Clare Fox
i think people are freakin out over like 10ms of qt prolongation like its a death sentence. my grandpa was on 40mg citalopram for 12 years, never had a problem, and now they want him to drop to 20 because some guy in a lab said ‘maybe?’ he could have a heart thing. he’s 82, walks 3 miles a day, eats kale. who’s the real risk here? the drug or the fear?
Akash Takyar
Thank you for this detailed and responsible analysis. In India, where access to ECG and electrolyte testing is limited, these guidelines are even more critical. Many patients are prescribed SSRIs without any cardiac evaluation-this can lead to preventable tragedies.
I have seen cases where patients on citalopram 40 mg developed syncope after starting diuretics. Had a baseline ECG been done, the risk could have been identified. We must advocate for low-cost, portable ECG devices in primary care clinics across developing nations.
Also, escitalopram’s lower risk profile makes it ideal for our context. Even if it costs more, the long-term savings in avoided hospitalizations justify it. Let us not confuse affordability with safety.
Finally, I urge all prescribers: when in doubt, choose lower dose, check electrolytes, and avoid combinations. A calm heart beats longer than a powerful one.
Arjun Deva
THIS IS A PHARMA COVER-UP. The FDA didn’t lower doses because of QT risk-they did it because they were bribed by Lundbeck to push escitalopram. Citalopram is generic. Escitalopram is brand. Same molecule, half the dose, double the price. They scared doctors into switching so they could keep profits alive.
And don’t tell me ‘the data shows’-the data was cooked. The original studies used flawed ECG machines. The QT measurements were biased. They cherry-picked the worst cases and ignored the 98% who were fine.
They want you to think you’re safe with 20mg. But what about the 10mg of escitalopram that’s actually 10.5mg because of ‘fillers’? The FDA doesn’t regulate those. The pills are made in China. Who knows what’s in them?
You think this is about health? It’s about control. They want you dependent on their expensive brand. They want you afraid to ask questions. They want you to trust the system… while they profit from your fear.
Inna Borovik
Let’s cut the pretense. This whole ‘QT prolongation’ scare is a glorified marketing campaign dressed up as science. The actual incidence of torsades from SSRIs? Less than 1 in 100,000 patient-years. You’re more likely to die from a lightning strike than from citalopram-induced arrhythmia.
Meanwhile, the real killers-obesity, smoking, sedentary lifestyles-are ignored because they’re too complex to fix with a pill or a dose cap.
And let’s not forget: the ‘safe’ alternatives like sertraline? They’ve got their own baggage. Sertraline causes more GI side effects, more sexual dysfunction, and more discontinuation syndrome. So we swap one risk for another and call it ‘better.’
This isn’t medicine. It’s risk theater. We’re treating depression like it’s a nuclear reactor. It’s not. It’s a broken mood circuit. And we’re treating it like a bomb.
Also-why is no one talking about the fact that antidepressants work better at higher doses for many people? We’re sacrificing efficacy on the altar of hypothetical risk. That’s not evidence-based. That’s fear-based.
Jackie Petersen
Why are we letting the government decide what’s safe for our hearts? This is America. I should be able to take whatever dose my doctor says I need. If I’m fine on 40mg of citalopram for 8 years, why should some bureaucrat in D.C. tell me to cut it in half? It’s not their body. It’s mine.
And why is escitalopram always the ‘better’ choice? Because it’s owned by a Danish company that lobbies hard. Citalopram’s made by a hundred generic labs. They don’t have the money to buy politicians. So they get punished.
Next they’ll ban ibuprofen because it ‘might’ raise blood pressure. Then they’ll ban coffee because caffeine ‘might’ affect QT. Next thing you know, we’re all on a 5mg daily antidepressant pill and told to meditate our way out of sadness.
This isn’t science. It’s socialism with a stethoscope.
Annie Gardiner
Actually, I think the real problem is that we’re still treating depression like it’s a chemical imbalance. Maybe the QT prolongation isn’t the danger-it’s the fact that we’re even using these drugs at all. Maybe the solution isn’t lower doses-it’s therapy, sunlight, movement, community.
But no-we’d rather stick a pill in someone’s mouth and call it a day. Then we get scared when the pill messes with their heart. We’re not fixing the problem. We’re just managing the symptoms… while ignoring the root causes.
And let’s be honest-most people on SSRIs aren’t on them because they’re clinically depressed. They’re on them because life sucks and they don’t know how to cope. We’re medicating existential dread with a drug that might kill you.
So yes-lower the dose. But also ask: why does anyone need this much of a chemical crutch in the first place?
Also-escitalopram at 10mg is just a placebo with a fancy label. I’ve seen people say they feel better after switching from citalopram to escitalopram… but their blood levels didn’t change. It’s the brand, not the biology.
Maybe we need to stop trusting pills and start trusting people.