DOAC Procedure Timing Calculator
Calculate Safe Dental Procedure Time
Enter your medication details to calculate safe procedure timing.
Important: This tool is for DOACs only. For warfarin, your dentist must check your INR level before any procedure.
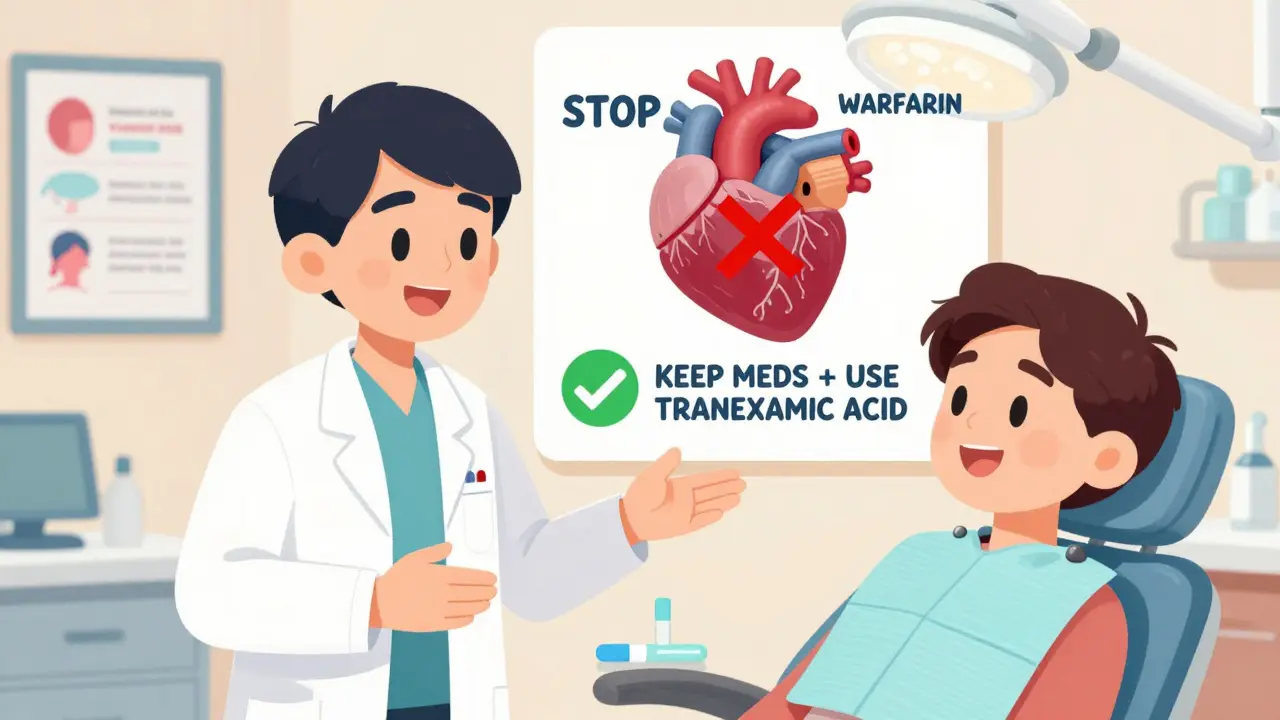
Why You Can’t Just Stop Your Blood Thinners Before a Dental Visit
Many people on blood thinners assume they need to pause their medication before a dental procedure. That’s a dangerous myth. Stopping anticoagulants like warfarin, Eliquis, or Xarelto for a simple filling or even a single tooth extraction doesn’t reduce bleeding risk-it increases the chance of a stroke, heart attack, or clot in your lungs. The data is clear: patients who stop their blood thinners for dental work are 3.5 times more likely to suffer a life-threatening clot than those who keep taking them.
Modern dental care doesn’t require you to choose between bleeding and clotting. It’s about managing both safely. Today’s protocols focus on keeping your medication going and using smart, targeted techniques to control bleeding right at the site. You don’t need to feel anxious about your next cleaning or extraction. With the right approach, it’s safer than ever.
Understanding Your Blood Thinner: Warfarin vs. DOACs
Not all blood thinners are the same. If you’re on warfarin, your dentist needs to check your INR level-a blood test that measures how long it takes your blood to clot. For most dental work, an INR under 3.5 is considered safe. If your INR is higher, your dentist might delay the procedure or ask your doctor to adjust your dose.
If you’re on a DOAC-like apixaban (Eliquis), rivaroxaban (Xarelto), or dabigatran (Pradaxa)-there’s no routine blood test. Instead, timing matters. These drugs clear from your system faster than warfarin. For a single tooth extraction, your dentist should wait at least 12 hours after your last dose of rivaroxaban, and 24 hours after your last dose if you take it twice daily. For apixaban, a 4-hour wait is usually enough. That’s because bleeding risk spikes if the drug is still at peak levels in your blood.
Here’s the key difference: warfarin needs monitoring. DOACs need timing. Both can be managed safely without stopping.
What Dental Procedures Are Safe With Blood Thinners?
You don’t need to avoid dental care. Most common procedures are low-risk even if you’re on anticoagulants.
- Low-risk procedures: Fillings, cleanings, root canals, simple extractions (one tooth), and local anesthetic injections. Bleeding rates here are under 3%. You keep your medication on.
- Moderate-risk procedures: Multiple extractions (2-4 teeth), gum surgery, or deep cleaning below the gumline. INR should be under 2.5 for warfarin patients. DOAC users should stick to the 12-24 hour window after their last dose.
- High-risk procedures: Full-mouth extractions, complex implant placements, or major jaw surgery. These require INR under 2.0 for warfarin patients and often a consultation with your cardiologist or hematologist.
Studies show that even with multiple extractions, bleeding complications stay below 6% when protocols are followed. The bigger danger isn’t the bleeding-it’s stopping your medicine.
How Dentists Control Bleeding Without Stopping Your Meds
Dentists aren’t just relying on pressure and gauze anymore. There are proven, powerful tools that work right at the site of bleeding.
- Tranexamic acid mouthwash: A 5% solution you rinse four times a day for a week after your procedure. It reduces bleeding by 62%. It’s cheap, safe, and doesn’t interfere with your blood thinner.
- Oxidized regenerated cellulose (Surgicel®): A dissolvable sponge placed directly into the extraction socket. It cuts bleeding time by nearly half compared to regular gauze.
- Microfibrillar collagen (Avitene®): This material attracts platelets and helps form clots fast. It works in over 92% of cases, even with high INR levels.
- Lidocaine with epinephrine: The local anesthetic your dentist uses isn’t just for numbness. The epinephrine (1:100,000 concentration) tightens blood vessels at the site, reducing bleeding by 32%.
These aren’t experimental. They’re standard tools in clinics that follow current guidelines. Your dentist should have at least two of these on hand before starting any procedure.

The Biggest Mistake Dentists Still Make
Despite clear guidelines, nearly half of U.S. dentists still tell patients to stop warfarin before extractions. A 2022 survey found 43.7% of dentists routinely discontinue anticoagulants for single-tooth removals-even though research shows this increases the risk of emergency hospital visits for clots by nearly 20%.
Why does this keep happening? Lack of training. Many dentists weren’t taught how to manage anticoagulants in school. Others fear lawsuits if a patient bleeds. But the data says the opposite: stopping the drug is riskier than letting it run.
If your dentist suggests stopping your blood thinner, ask: “What’s the plan to prevent a stroke?” If they can’t answer, get a second opinion. You have the right to care based on current evidence, not outdated habits.
What You Should Do Before Your Appointment
Don’t wait until the day of your appointment to figure this out. Take control.
- Know your medication: Write down the name, dose, and when you last took it. If you’re on warfarin, know your last INR result.
- Call your doctor: Ask if your current dose is safe for dental work. For DOACs, ask: “Is it okay to proceed if I haven’t taken my pill in the last 12 hours?”
- Bring your records: Take a copy of your most recent INR result or your DOAC prescription. Many dentists don’t have access to your medical history.
- Ask about hemostatic tools: Don’t be shy. Ask: “Will you use tranexamic acid or Surgicel®?” If they say no, find a dentist who does.
These steps take 10 minutes. They could save your life.
Pain Relief After: What to Take (and What to Avoid)
After your procedure, pain relief is important-but some common meds can be dangerous.
Avoid: Ibuprofen, naproxen, aspirin (unless it’s your prescribed heart medication). These NSAIDs increase bleeding risk 3-6 times when combined with anticoagulants.
Use: Acetaminophen (Tylenol). It’s safe for most patients. But if you take more than 2,000 mg a day for over a week, ask your doctor to check your INR. High doses can slightly affect how warfarin works.
Antibiotics matter too. Metronidazole (Flagyl) can boost warfarin’s effect, raising your INR dangerously. If you need antibiotics, ask for azithromycin instead-it doesn’t interfere.

What’s New in 2026: Faster Testing and Better Tools
Technology is making anticoagulant management easier than ever. Portable INR monitors like CoaguChek® let dentists test your blood right in the chair. Results in 60 seconds. No more waiting days for lab reports.
Reversal agents are improving too. Andexxa® can reverse DOACs in emergencies, though it’s expensive and only used in life-threatening bleeding. New topical gels with recombinant factor VIIa are being tested and show promise for high-risk patients.
AI tools are also emerging. One system at the University of Pennsylvania predicts bleeding risk with 89% accuracy by analyzing your age, INR, procedure type, and other factors. Dentists won’t rely on guesswork much longer.
Final Rule: Never Stop Your Blood Thinner Without a Doctor’s Say
There’s one rule that never changes: never stop your anticoagulant for a dental procedure unless your cardiologist or hematologist tells you to. Bridging with heparin? It’s outdated and dangerous. Studies show it triples bleeding risk without preventing clots.
The best outcome isn’t zero bleeding. It’s zero stroke. You can have both-when you work with a dentist who knows the science.
When to See a Specialist
Not every dentist is experienced with complex anticoagulant cases. You should be referred to an oral surgeon or dental anesthesiologist if:
- You have a mechanical heart valve, especially in the mitral position
- Your INR is above 3.5 and can’t be lowered safely
- You’re on dual antiplatelet therapy (aspirin + clopidogrel)
- You’ve had a recent stroke, heart attack, or pulmonary embolism in the last 3 months
These cases need a team approach. Don’t hesitate to ask for a referral.

Claire Wiltshire
Thank you for this incredibly clear and evidence-based breakdown. As a dental hygienist with 18 years in practice, I’ve seen too many patients harmed by outdated protocols. The data on clot risk versus bleeding is unequivocal, and it’s our responsibility to educate both patients and colleagues. Tranexamic acid mouthwash alone has transformed our post-op outcomes-cheap, effective, and safe. If your dentist still recommends stopping anticoagulants, they’re operating on memory, not medicine.
Darren Gormley
LMAO 🤡 so now we’re supposed to trust dentists with our lives? Next they’ll say ‘just don’t breathe’ during a root canal. I got my tooth pulled last year, stopped my Eliquis for 3 days, and guess what? I didn’t die. Also, who the hell uses Surgicel® anymore? That’s 2008 tech. 🤷♂️
Mike Rose
idk man i just got a filling and my dentist told me to skip my blood thinner for a day. i did it and nothing happened. so maybe this whole thing is just fearmongering? i mean, i’m not a doctor but i know what happened to me.
Niamh Trihy
This is one of the most balanced and clinically accurate summaries I’ve read on this topic. The distinction between warfarin and DOACs is critical, and too many providers conflate them. I appreciate the specific timing recommendations-12 hours for rivaroxaban, 4 for apixaban. That’s actionable. Also, the point about epinephrine in local anesthetic is often overlooked. It’s not just for numbness-it’s hemostatic. Well done.
Yanaton Whittaker
AMERICA IS THE ONLY COUNTRY THAT DOES THIS RIGHT. In Europe they’re still using horsehair and vinegar for dental care. We have AI predicting bleeding risk? That’s innovation. That’s freedom. That’s what happens when you don’t have government-run healthcare telling dentists what to do. #MakeDentistryGreatAgain 🇺🇸
Natasha Plebani
The epistemological tension here lies in the conflation of procedural risk with systemic risk. The medical-industrial complex has weaponized statistical abstraction to normalize invasive intervention while pathologizing patient autonomy. The real danger isn’t bleeding-it’s the normalization of pharmacological dependency as a substitute for physiological resilience. We must interrogate why we prioritize clot prevention over hemostatic agency. Is this medicine-or control?
Kimberly Reker
I’m so glad this exists. I was terrified to get my wisdom teeth out because I’m on Xarelto. My dentist used tranexamic acid and didn’t make me stop my meds. I bled a little for a day, but zero clots, zero panic. Seriously, if you’re scared-ask about the mouthwash. It’s magic. And your dentist should have it. If they don’t, find one who does. You got this 💪
Eliana Botelho
Okay but why are we even talking about this like it’s a new thing? I’ve been on warfarin since 2015 and every dentist I’ve ever had told me to stop. I even had a doctor tell me to stop it before a tooth extraction. And guess what? I didn’t die. And now you’re telling me I was wrong? But my dentist said it was standard. And my cousin did the same thing and she’s fine. So why are you acting like this is the first time anyone’s ever heard of this? I’m just confused. Like, why now? Why this article? Why not before?
calanha nevin
The data is unequivocal. Stopping anticoagulants for dental procedures increases thrombotic events by 350 percent. This is not a suggestion. It is a clinical imperative. Your dentist must be informed. Your records must be provided. Your safety is non-negotiable. Do not defer. Do not assume. Act.
owori patrick
This is very helpful. I’m from Nigeria and we don’t have many dentists who understand anticoagulants. I shared this with my local clinic and they’re now ordering tranexamic acid. Thank you for writing this. We need more of these guides in low-resource settings. Knowledge should not be a privilege.
Sazzy De
I’ve been on Eliquis for 5 years and never stopped it for dental work. My dentist uses Surgicel and I’ve never had a problem. Just tell them you’re on it and they’ll figure it out. Easy.
Jodi Olson
The reliance on technological solutions like portable INR monitors and AI risk predictors reflects a deeper cultural shift-away from patient-centered clinical judgment and toward algorithmic certainty. We are not data points. We are humans with histories, fears, and bodies that do not always conform to statistical norms. The real innovation is not in the machine-it is in the clinician who listens.
Carolyn Whitehead
this made me feel so much better about my cleaning next week. i was nervous but now i know what to ask for. thanks for the tips on the mouthwash and acetaminophen. i’m gonna print this out and take it with me 🙏
Katie and Nathan Milburn
The assertion that stopping anticoagulants increases thrombotic risk by 3.5 times is statistically robust and corroborated by multiple meta-analyses, including the 2021 Cochrane Review on dental anticoagulation management. However, the clinical application remains inconsistent due to fragmented continuing education and liability aversion. The solution lies not in individual patient advocacy alone, but in institutional mandates requiring standardized protocols and mandatory continuing education for all licensed dental practitioners.