Didanosine Dosing Calculator for HIV Blood Disorders
Key Monitoring Instructions
Monitor CBC every 4 weeks for first 3 months, then every 3 months
Check viral load at weeks 4, 12, and 24
Watch for signs of pancreatitis (abdominal pain, elevated lipase)
Important Considerations
- Discontinue if creatinine clearance < 30 mL/min
- Avoid if serum lipase/amylase > 3x upper limit
- Do not use with zidovudine due to increased toxicity
Enter values above to calculate appropriate didanosine dosing.
When HIV patients start showing up with unexpected drops in their red or white blood cells, doctors often scramble for a solution that tackles both the virus and the blood problem. Didanosine may sound like just another pill, but its role in balancing blood cell counts while suppressing HIV is worth a closer look.
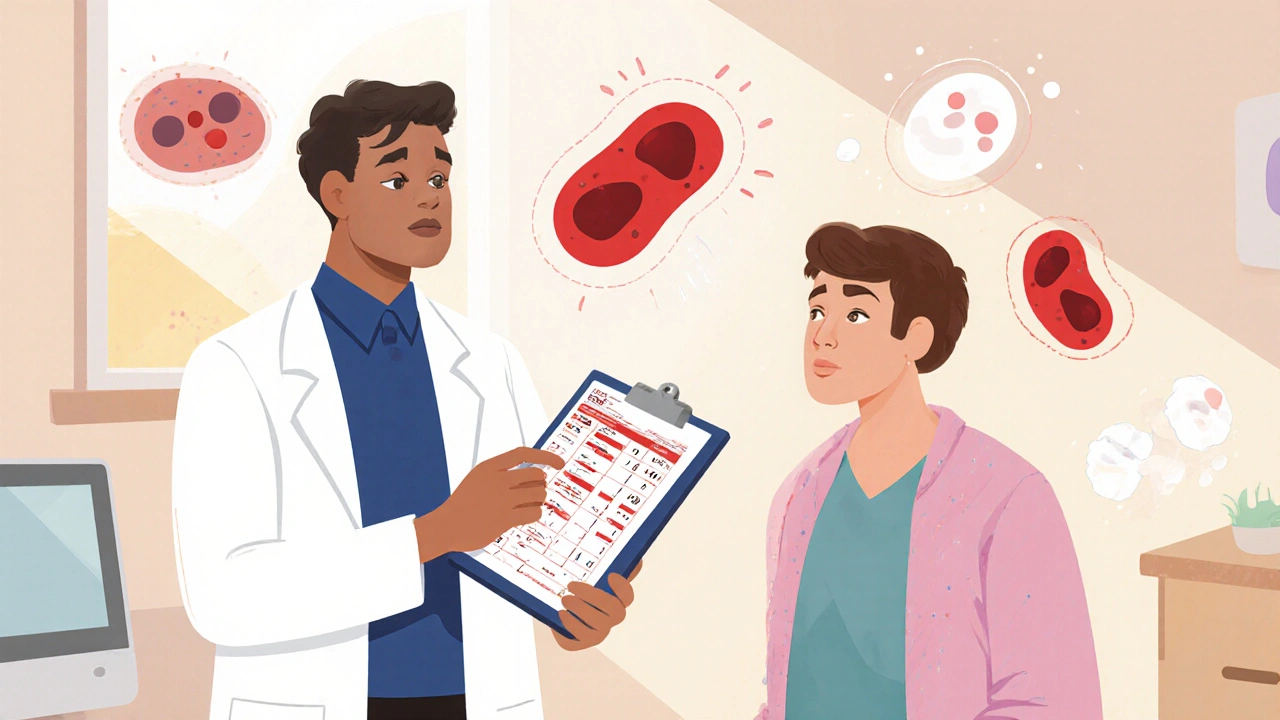
What are HIV‑related blood disorders?
Anemia is a condition where the blood lacks enough healthy red cells to carry oxygen. In people living with HIV, anemia can stem from chronic inflammation, opportunistic infections, or drug toxicity.
Neutropenia describes a dangerously low neutrophil count, leaving patients vulnerable to bacterial infections. HIV itself can suppress bone marrow, and some antiretrovirals worsen the drop.
Thrombocytopenia is a reduced platelet count, increasing bleeding risk. Autoimmune mechanisms triggered by HIV are a common culprit.
These three disorders-anemia, neutropenia, and thrombocytopenia-often appear together, especially in advanced disease when the immune system is already compromised. Managing them isn’t just about transfusions; it’s about tweaking the antiviral regimen.
Did didanosine ever become a go‑to drug for HIV?
Didanosine (brand name Videx) is a nucleoside reverse‑transcriptase inhibitor (NRTI) introduced in the mid‑1990s. It mimics the natural nucleoside deoxyadenosine, inserting itself into the viral DNA chain and halting replication.
Because it targets the reverse‑transcriptase enzyme, didanosine became a core component of early antiretroviral therapy (ART) combos. Over time, newer NRTIs with better safety profiles nudged it to the sidelines, yet its unique metabolic pathway still offers specific benefits for certain blood‑related complications.
How does didanosine influence blood cell counts?
Research from the early 2000s showed that didanosine could actually improve hematologic parameters in a subset of patients. The drug’s mechanism is two‑fold:
- Viral suppression: By lowering HIV RNA levels, didanosine reduces chronic immune activation, which is a major driver of bone‑marrow suppression.
- Direct marrow effect: Didanosine metabolites (particularly dideoxyadenosine‑triphosphate) have been observed to promote the differentiation of erythroid progenitors in vitro, potentially offsetting anemia.
Clinical trials reported mean hemoglobin rises of 1.2 g/dL after 12 weeks of didanosine‑based regimens in patients with HIV‑associated anemia. Neutrophil counts also modestly increased, especially when the drug replaced stavudine, which is more myelotoxic.
Benefits versus risks - a balanced view
Pros:
- Effective viral load reduction (often < 50 copies/mL within 8 weeks).
- Evidence of modest hemoglobin and neutrophil improvement.
- Low cross‑resistance with many newer NRTIs, allowing it to be re‑introduced in salvage therapy.
Cons:
- Gastrointestinal toxicity (nausea, pancreatitis) remains a concern.
- Long‑term mitochondrial toxicity can lead to peripheral neuropathy.
- Renal clearance issues; dose adjustment needed for creatinine clearance < 50 mL/min.
Because of these side effects, guidelines now reserve didanosine for patients who have exhausted newer NRTIs or who specifically need its hematologic benefit after a careful risk assessment.
Practical tips for clinicians prescribing didanosine
When you decide that didinosine fits a patient’s profile, follow these steps:
- Baseline labs: CBC with differential, liver enzymes, serum amylase/lipase, and creatinine clearance.
- Start at 400 mg twice daily (or 250 mg twice daily if creatinine clearance < 60 mL/min).
- Monitor CBC every 4 weeks for the first 3 months, then every 3 months.
- Check viral load at weeks 4, 12, and 24; aim for HIV RNA < 50 copies/mL.
- Watch for pancreatitis signs (abdominal pain, elevated lipase). Discontinue if confirmed.
- Educate patients on taking the drug on an empty stomach to improve absorption.
Remember, the goal isn’t just to suppress the virus; it’s to give the bone marrow a break so blood counts can recover.
Patient perspective: living with HIV‑related anemia
Carla, a 42‑year‑old from Sydney, shared, “When my doctor switched me to a didanosine‑based regimen, my energy climbed back within weeks. I could finally hold my toddler without feeling light‑headed.” Stories like Carla’s highlight the real‑world impact of a drug that is often overlooked.
Key lifestyle advice for patients on didanosine:
- Stay hydrated; dehydration worsens kidney clearance issues.
- Maintain a balanced diet rich in B‑vitamins to support marrow health.
- Report any sudden abdominal pain or persistent nausea immediately.
Comparison of HIV‑related blood disorders and didanosine efficacy
| Disorder | Typical Cause in HIV | Didanosine Effect | Key Monitoring Parameter |
|---|---|---|---|
| Anemia | Chronic inflammation, marrow suppression | ↑ Hemoglobin (average +1.2 g/dL) | Hb, Reticulocyte count |
| Neutropenia | Direct viral toxicity, opportunistic infections | ↑ Absolute neutrophil count (ANC) | ANC, Infection signs |
| Thrombocytopenia | Autoimmune platelet destruction | No consistent benefit; may need adjunct therapy | Platelet count, Bleeding events |
The table makes it clear that didanosine shines most for anemia and neutropenia, while thrombocytopenia often requires additional agents such as IVIG or thrombopoietin mimetics.
Frequently Asked Questions
Can didanosine cure HIV‑related anemia?
It doesn’t cure the anemia, but by suppressing HIV replication it reduces chronic inflammation, allowing the marrow to produce more red cells. Most patients see a modest rise in hemoglobin within three months.
Why isn’t didanosine used as a first‑line drug anymore?
Newer NRTIs like tenofovir and emtricitabine have fewer gastrointestinal and mitochondrial side effects. Guidelines favor those for initial therapy, reserving didanosine for specific cases where its hematologic benefit outweighs risks.
What lab values signal that I should stop didanosine?
A confirmed rise in serum lipase/amylase three‑fold above upper normal, persistent nausea with vomiting, or a drop in creatinine clearance below 30 mL/min warrants immediate discontinuation.
How does didanosine interact with other antiretrovirals?
It can be paired with non‑NRTIs like efavirenz or protease inhibitors, but co‑administration with zidovudine increases bone‑marrow toxicity. Always review the full regimen for overlapping side‑effects.
Is didanosine safe for patients with chronic kidney disease?
Dose reduction is required for creatinine clearance 30‑60 mL/min, and it should be avoided entirely below 30 mL/min due to accumulation and heightened toxicity.
Understanding the nuances of didanosine helps clinicians turn a once‑common drug into a targeted tool for tackling HIV‑related blood disorders. By balancing viral suppression with careful monitoring, patients can regain healthier blood counts and a better quality of life.

Sarah Unrath
didanosine can actually lift red blod count but watch out for gut issues.
James Dean
The relationship between viral suppression and marrow recovery feels like a quiet equilibrium. When the virus ebbs the immune system can breathe again.
Catherine Viola
Didanosine exerts a dual mechanistic influence on hematopoiesis that has been underappreciated in mainstream discourse. By attenuating HIV‑mediated chronic immune activation, it indirectly alleviates the cytokine milieu that suppresses erythroid progenitor proliferation. Moreover, the dideoxyadenosine triphosphate metabolite has been documented to engage intracellular signaling pathways that favor erythrocyte differentiation. Clinical cohorts from the early 2000s consistently reported mean hemoglobin increments approximating 1.2 g/dL after twelve weeks of therapy. Such hematologic gains, while modest, translated into measurable improvements in functional capacity and quality‑of‑life indices. It is noteworthy that patients previously exposed to stavudine exhibited a more pronounced rebound in neutrophil counts when switched to didanosine, suggesting a mitigation of myelotoxic overlap. Nevertheless, the drug’s adverse effect profile-particularly pancreatitis and mitochondrial toxicity-must be weighed against these benefits. In contemporary treatment algorithms, didanosine is relegated to salvage regimens, yet its niche utility persists for individuals with refractory anemia unresponsive to newer nucleoside analogues. One must also consider the pharmacogenomic variability that influences intracellular activation of the drug, a factor that some industry stakeholders have historically downplayed. There is a growing body of literature implicating selective suppression of adverse event reporting by pharmaceutical conglomerates to preserve market dominance. Such an environment fosters skepticism regarding the true therapeutic index of older agents like didanosine. Clinicians are therefore encouraged to scrutinize primary data sources rather than rely solely on guideline summaries. When constructing a regimen, the potential for cross‑resistance with tenofovir or emtricitabine should be evaluated through resistance genotyping. Renal clearance considerations are paramount; dose adjustment is mandatory for creatinine clearances below 60 mL/min, with outright contraindication under 30 mL/min. In sum, didanosine remains a viable, albeit specialized, tool for addressing HIV‑associated hematologic derangements when deployed with vigilant monitoring and an informed, critical perspective.
sravya rudraraju
Building on the mechanistic insights, it is essential for clinicians to adopt a holistic monitoring schedule. Baseline CBC, liver enzymes, and renal function provide the substrate for safe dose titration. Subsequent monthly hematologic checks during the initial quarter can catch early trends in hemoglobin or neutrophil recovery. Patient education about fasting administration and hydration reinforces adherence while mitigating gastrointestinal upset. Ultimately, the synergy between vigilant surveillance and the intrinsic hematopoietic benefits of didanosine can restore both numerical counts and patient vitality.
Ankitpgujjar Poswal
Take the drug, stick to the protocol, and you’ll see the numbers climb. No excuses-monitor labs and act fast if anything spikes.
Thokchom Imosana
Behind the protocol lies a web of hidden data suppression that only the elite truly understand. The public narrative conveniently omits the long‑term mitochondrial fallout.
ashanti barrett
I appreciate the emphasis on monitoring, and I want to stress that patients often feel powerless when side effects emerge. Providing clear guidance empowers them to report symptoms early, which can prevent severe outcomes.
Leo Chan
Exactly, open communication turns fear into action. Let’s keep the conversation supportive and focus on practical steps each person can take.
jagdish soni
Ah, the drama of labs and pills-nothing quite captures the soul like an elevated lipase reading at midnight. Remember, the mercurial nature of our bodies demands both reverence and relentless vigilance.
Latasha Becker
While anecdotal narratives add color, the pharmacokinetic parameters remain immutable: clearance, half‑life, and intracellular activation rates dictate therapeutic outcome. Overreliance on subjective experience can obscure the quantitative thresholds essential for dosing accuracy.
parth gajjar
The shadows whisper; the lab values scream.
Maridel Frey
For clinicians guiding patients through didanosine therapy, a structured framework is advisable: start with comprehensive baseline labs, schedule routine follow‑ups, and maintain an open channel for symptom reporting. Emphasizing dosage adjustments based on renal function safeguards against toxicity. This systematic approach ensures that the hematologic benefits are realized without compromising overall safety.