NSAID Comparison Tool
Find Your Ideal NSAID
Answer a few questions to see which NSAIDs match your health profile
Matching NSAIDs
When you’re battling joint pain or a flare‑up of arthritis, the first question that pops up is: *which NSAID will give me relief without a laundry list of side effects?* Etodolac is a popular option, but it’s not the only player on the field. This guide breaks down what Etodolac does, how it stacks up against its rivals, and how to choose the right medication for your lifestyle.
What Is Etodolac?
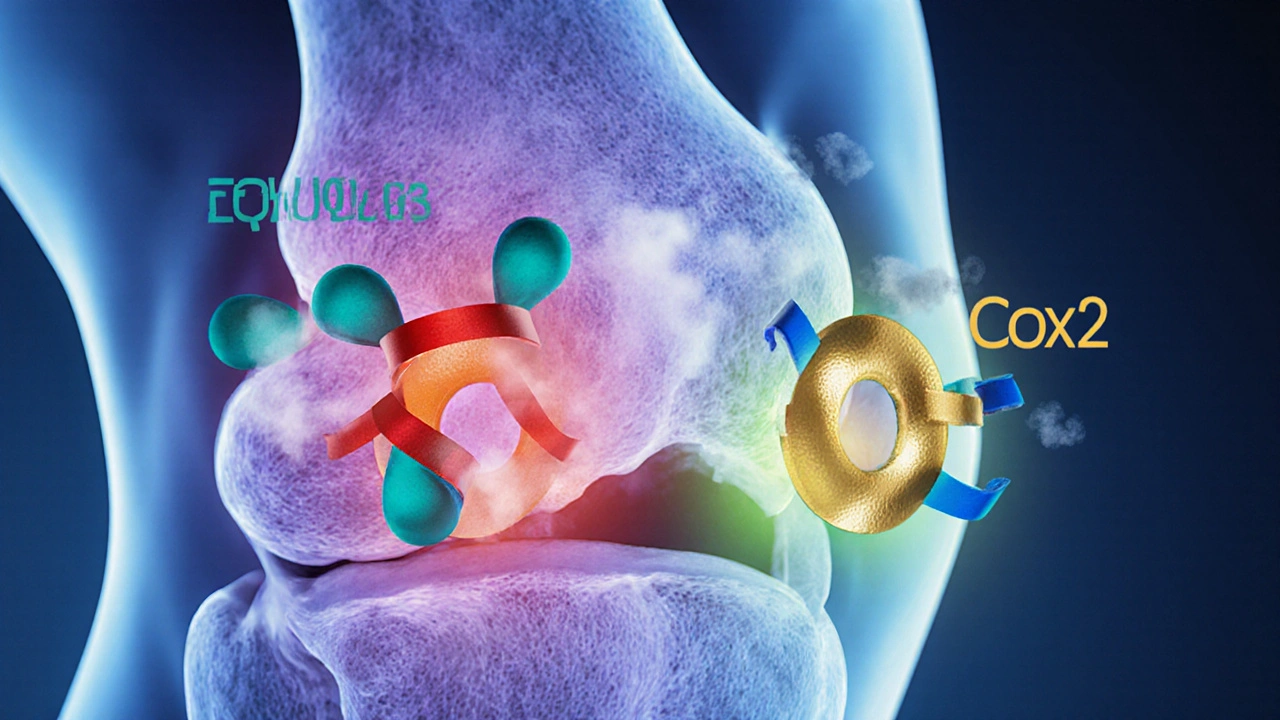
Etodolac is a prescription non‑steroidal anti‑inflammatory drug (NSAID) that works by inhibiting cyclooxygenase‑2 (COX‑2), the enzyme responsible for producing prostaglandins that cause pain and swelling. It’s approved for osteoarthritis, rheumatoid arthritis, and acute musculoskeletal pain. Typical adult dosing starts at 300mg once daily or 200mg twice daily, with a half‑life of about 6‑7hours, allowing for twice‑daily dosing for most patients. Common side effects include stomach upset, headache, and mild dizziness, while rare but serious risks involve gastrointestinal bleeding, cardiovascular events, and elevated liver enzymes.
Top NSAID Alternatives to Consider
Below are the most frequently prescribed NSAIDs that doctors compare with Etodolac. Each entry includes a brief snapshot of its pharmacology, typical dosing, and safety profile.
- Naproxen is a longer‑acting NSAID that blocks both COX‑1 and COX‑2, offering up to 12hours of pain relief. Standard adult dose is 250‑500mg twice daily. It carries a moderate risk of GI irritation but a lower cardiovascular risk than some selective COX‑2 inhibitors.
- Ibuprofen is an over‑the‑counter NSAID that inhibits COX‑1 and COX‑2 with a rapid onset. Typical doses range from 200‑400mg every 4‑6hours, not exceeding 3200mg per day. It’s gentle on the stomach for short‑term use but can raise blood pressure in sensitive individuals.
- Diclofenac is a potent NSAID often used for severe inflammatory conditions. The usual oral dose is 50‑75mg two to three times daily. It is associated with higher cardiovascular risk, so clinicians reserve it for patients without heart disease.
- Celecoxib is a selective COX‑2 inhibitor marketed under the brand name Celebrex. It provides 12‑hour pain control at 200‑400mg once daily and tends to cause fewer stomach ulcers, but it carries a clear warning for increased risk of heart attack and stroke.
- Indomethacin is a strong NSAID used mainly for gout and ankylosing spondylitis. Dosing starts at 25‑50mg two to three times daily. It can be harsh on the gastrointestinal tract and may cause central nervous system side effects like mood changes.
- Aspirin (acetylsalicylic acid) is the original NSAID, low‑dose (81mg) for cardioprotection and higher doses (325‑650mg) for pain. Its antiplatelet effect makes it unsuitable for combination with many other NSAIDs because of bleeding risk.
Side‑by‑Side Comparison
| Drug | Typical Adult Dose | Half‑Life | COX Selectivity | GI Risk | Cardiovascular Risk | Average Monthly Cost (USD) |
|---|---|---|---|---|---|---|
| Etodolac | 300mg once daily or 200mg twice daily | 6‑7h | COX‑2 > COX‑1 (moderate selectivity) | Moderate | Low‑moderate | $15‑$25 |
| Naproxen | 250‑500mg twice daily | 12‑17h | Non‑selective (COX‑1 & COX‑2) | Moderate | Low | $10‑$20 |
| Ibuprofen | 200‑400mg every 4‑6h (max 3200mg/d) | 2‑4h | Non‑selective | Low‑moderate | Low | $5‑$15 |
| Diclofenac | 50‑75mg 2‑3×/day | 1‑2h | Non‑selective | Low‑moderate | High | $20‑$30 |
| Celecoxib | 200‑400mg once daily | 11‑12h | Highly COX‑2 selective | Low | High | $25‑$45 |
| Indomethacin | 25‑50mg 2‑3×/day | 4‑5h | Non‑selective | High | Moderate | $15‑$25 |
| Aspirin | 81mg daily (cardio) or 325‑650mg q4‑6h (pain) | 15‑20min (platelet effect lasts 7‑10days) | COX‑1 irreversible inhibitor | High (ulcer risk) | Low (cardio‑protective at low dose) | $2‑$8 |
How to Choose the Right NSAID for Your Situation
Picking a pain reliever isn’t a one‑size‑fits‑all decision. Consider these three axes:
- GI safety. If you have a history of ulcers or are on anticoagulants, a COX‑2‑selective agent like Celecoxib may spare your stomach, but keep an eye on heart health.
- Cardiovascular profile. Patients with hypertension, prior heart attack, or stroke should steer clear of drugs with high CV risk (e.g., diclofenac, celecoxib). Etodolac and naproxen sit on the safer side.
- Duration of pain. For short‑term flare‑ups, ibuprofen’s rapid onset works well. For chronic arthritis needing steady control, naproxen or etodolac’s twice‑daily dosing offers more consistent relief.
Age, kidney function, and concurrent medications also shape the choice. Always run a quick check with your clinician before swapping drugs.

Switching From Etodolac to Another NSAID
If your doctor suggests a switch-say, from Etodolac to naproxen-follow these steps to avoid gaps in pain control and minimize side‑effects:
- Complete the current Etodolac pack unless advised otherwise.
- Start the new NSAID at the lowest effective dose (e.g., naproxen 250mg twice daily).
- Take the new medication with food to protect the stomach.
- Monitor for any new symptoms such as bruising, swelling, or stomach pain for the first 2 weeks.
- Schedule a follow‑up visit to assess pain relief and any lab changes (especially kidney function).
Never combine two NSAIDs; the risk of GI bleeding and kidney injury spikes dramatically.
Key Takeaways
- Etodolac delivers moderate pain relief with a balanced GI and cardiovascular risk profile.
- For longer‑lasting relief, naproxen is a solid OTC option; for rapid, short‑term pain, ibuprofen works best.
- Patients with heart disease should avoid high‑risk NSAIDs like diclofenac and celecoxib.
- Switching NSAIDs is safe when you taper the old drug and start the new one at a low dose with food.
- Always discuss your full medical history with a healthcare provider before starting or changing any NSAID.
Frequently Asked Questions
Can I take Etodolac and ibuprofen together?
No. Combining two NSAIDs raises the chance of stomach bleeding, kidney problems, and high blood pressure. If you need extra pain control, ask your doctor about switching rather than stacking.
Is Etodolac safe for people over 65?
Older adults are more prone to GI ulcers and kidney decline. Etodolac can be used if the dose is low and a gastro‑protective agent (like a proton‑pump inhibitor) is added. Always get a doctor’s clearance.
How does naproxen compare to etodolac for arthritis?
Naproxen has a longer half‑life (12‑17h) so you usually take it twice daily, while etodolac is taken once or twice daily. Both have moderate GI risk, but naproxen shows the lowest cardiovascular risk of the group, making it a good first‑line OTC choice for many arthritis patients.
Why would a doctor prescribe celecoxib instead of etodolac?
Celecoxib is highly COX‑2 selective, so it causes fewer stomach ulcers. Doctors may pick it for patients with a strong ulcer history who can tolerate the higher cardiovascular warning, especially if the patient needs once‑daily dosing.
What lab tests should I get while on an NSAID?
Baseline and periodic checks of kidney function (creatinine, eGFR), liver enzymes (ALT, AST), and complete blood count are advisable. If you have a history of heart disease, your doctor might also monitor blood pressure and lipid profile.


Bailee Swenson
Etodolac gets a lot of hype, but it’s really just a middle‑of‑the‑road NSAID that most people can live without. If you’re chasing the “COX‑2‑selective” label, you might as well read the label on celecoxib. The GI risk is labeled moderate, yet you’ll find the same ulcer rates with ibuprofen if you don’t protect the stomach. Cardiovascularly, Etodolac sits somewhere between naproxen’s safety and diclofenac’s nightmare. For a $20‑$30 monthly bill, you’re paying for nothing spectacular. Most clinical guidelines place naproxen as the first‑line OTC choice for arthritis. If you can’t tolerate naproxen, ibuprofen is a tried‑and‑tested fallback. Switching from Etodolac to a COX‑2‑selective drug just trades GI risk for a higher heart‑attack risk. The half‑life of 6‑7 hours means you’re still dosing twice a day, no convenience win. And let’s not forget the drug interactions – mixing Etodolac with antihypertensives can blunt their effect. Patients over 65 should be on a proton‑pump inhibitor if they even think about using Etodolac. The data on liver toxicity is sparse, but you’ll still need periodic labs. Bottom line: unless your rheumatologist specifically prefers it, you’re better off with a cheaper, safer option. Don’t be fooled by the “prescription‑only” badge; it’s a marketing ploy. 💊🚫
tony ferreres
When you weigh Etodolac against its peers, think of it as a middle‑ground philosopher-neither the bold rebel nor the timid pacifist. 🌿 Its COX‑2 tilt offers a modest GI safety boost, but the cardiovascular cost remains a whisper in the background. For many, naproxen’s longer half‑life feels like a steady meditation, while ibuprofen’s quick onset is a flash of insight. The key is matching the drug’s rhythm to your body’s cadence, not chasing the flashiest label. 🎯 A low‑cost, low‑risk regimen often beats a prescription‑only hype train. Remember, the best choice respects both the science and your daily routine.
Kaustubh Panat
One must contemplate the ontological hierarchy of NSAIDs before bestowing any mortal with Etodolac’s modest accolades.
Arjun Premnath
I hear your concerns about Etodolac’s risk profile, and they’re certainly valid. While the drug does sit in a moderate zone for GI irritation, many patients tolerate it well with a proton‑pump inhibitor. It’s crucial to individualize therapy based on comorbidities, especially in the elderly. A shared decision‑making approach can help balance efficacy and safety. Ultimately, the clinician’s guidance remains the cornerstone of any NSAID regimen.
Johnny X-Ray
Wow, this is like a blockbuster showdown of pain meds! 🎬💥 I’m all for finding the perfect hero drug, and sometimes Etodolac can be the underdog that surprisingly saves the day. But if you want a reliable star, naproxen often gets the standing ovation. Keep the drama low and the relief high, folks! 😊
Molly Beardall
Honestly, the whole Etodolac debate feels like a soap opera with too many plot twists. The data tables are clear, yet people keep re‑writing the script, ignoring the fact that diclofenac’s CV risk is off the charts. It’s almost comical how some prescribers chase brand names while discounting basic pharmacology. Is anyone else seeing the same far‑cetched arguments, or am I just being dramatic? I definitly think we need to stick to the numbers.
Elijah Mbachu
Man, that was a deep take! Even if Etodolac isn’t the top dog, it still has its place in the toolkit. Just make sure you check kidney function before you start, especially if u’re on other meds. Keep it simple and stay safe.
Sunil Rawat
Hey folks! If you’re looking for an NSAID that’s easy on the stomach, celecoxib might be worth a look, but remember it can stress the heart. For most everyday aches, ibuprofen does the job and is cheap. Stay healthy!
Andrew Buchanan
Your observation about the over‑emphasis on brand names is spot‑on. When evaluating NSAIDs, the primary endpoints should be efficacy, GI safety, and cardiovascular risk, not marketing hype. Evidence‑based guidelines consistently place naproxen and ibuprofen near the top for balance. It’s essential to communicate these data clearly to patients.
Jonathan Martens
From a pharmacoeconomic perspective, Etodolac offers marginal incremental cost‑effectiveness in a niche cohort, but the ROI is dubious. Unless you’re conducting a head‑to‑head RCT, the data pool is thin. TL;DR: pick the drug with the best safety‑efficacy profile, not the flashiest label.
Jessica Davies
Actually, the whole notion that Etodolac is “moderate” is a myth propagated by pharmaceutical PR. The GI bleed rates are comparable to high‑risk agents, and the cardiovascular warnings are understated. I’d steer clear unless you have no other options.
Kyle Rhines
It is imperative to verify the primary literature before accepting any claim about NSAID safety. Many sources cited online are either outdated or selectively quoted, possibly due to undisclosed industry funding. Patients should request original peer‑reviewed studies rather than rely on secondary summaries.
Lin Zhao
Great point! 📚 I always try to dig into the original papers myself – it feels empowering. If anyone needs a quick guide to reputable journals on NSAIDs, just shout out. 😊