Anticholinergic Burden Calculator
How It Works
This calculator estimates your anticholinergic burden using the article's research on first-generation antihistamines. Each medication contributes to your cumulative risk score:
- High-risk: Diphenhydramine (Benadryl), Promethazine (Phenergan) - 1 point
- Medium-risk: Chlorpheniramine (Chlor-Trimeton), Hydroxyzine (Atarax) - 0.5 points
- Age adjustment: +0.5 points for users over 65
Take a diphenhydramine tablet for allergies, and you might feel better-but you’ll also feel drained. Not just tired. Heavy. Like your brain is wrapped in cotton. That’s not a side effect you can ignore. It’s the core trade-off of first-generation antihistamines: quick relief at the cost of mental clarity, coordination, and sometimes, long-term brain health.
How These Drugs Work-and Why They Make You Sleepy
First-generation antihistamines like diphenhydramine (Benadryl), chlorpheniramine (Chlor-Trimeton), promethazine (Phenergan), and hydroxyzine (Atarax) were developed in the 1940s. They block histamine, the chemical your body releases during allergic reactions. But here’s the catch: they don’t stop at the nose or skin. These drugs slip easily through the blood-brain barrier because they’re small and fat-soluble. Once inside the brain, they bind to H1 receptors in areas that control wakefulness, attention, and memory. This isn’t just mild sleepiness. Studies show these medications cause brain concentrations 15 to 25 nanograms per milliliter after a standard dose-enough to disrupt normal neural activity. In driving simulators, users perform as poorly as people with a blood alcohol level of 0.05%. That’s legally impaired in many countries. The effect doesn’t fade after a few hours. For some, brain fog lasts up to 18 hours.The Anticholinergic Domino Effect
These drugs don’t just mess with histamine. They also block muscarinic receptors-the same ones targeted by nerve agents and certain poisons. That’s why you get dry mouth, blurry vision, constipation, and trouble peeing. These are classic anticholinergic effects. And they’re not harmless quirks. They’re signs your nervous system is being overpowered. In older adults, this is especially dangerous. The American Geriatrics Society lists first-generation antihistamines as potentially inappropriate for people over 65. Why? Chronic use increases dementia risk by 54%. That’s not a small jump. It’s a clear signal: these drugs are building up in the brain, quietly damaging cognitive pathways. Even low doses taken nightly for sleep can add up. One study found 42% of elderly users still felt confused and disoriented hours after waking.Why People Still Use Them
If they’re this risky, why are they everywhere? Because they’re cheap, easy to get, and work fast. A bottle of 24 Benadryl tablets costs under $5. Compare that to $15 for a month’s supply of cetirizine or loratadine. For someone with occasional allergies or trouble falling asleep, the price is tempting. They’re also effective for motion sickness and nausea-far better than second-generation options. That’s why they’re still in many travel kits and used by cruise passengers. And for short-term insomnia, they work. They reduce sleep onset time by 30 to 40 minutes. But here’s the problem: they don’t improve sleep quality. You fall asleep faster, but you wake up groggy, with poor memory consolidation and disrupted REM cycles.
Real People, Real Consequences
Look at user reviews. On Drugs.com, 38% of people who took diphenhydramine reported “extreme sleepiness.” One Reddit user wrote: “Took Benadryl at 8 PM for hives. Woke up at 2 PM the next day like I’d been hit by a truck.” That’s not an exaggeration. It’s a documented pattern. Emergency rooms see the fallout. In 2021, 35% of drowsy driving incidents linked to medication involved first-generation antihistamines. People think, “I took it last night, I’m fine now.” But cognitive impairment lingers. A 2022 JAMA study found 45% of users underestimated how long the effects lasted. And it’s not just adults. Between 2018 and 2022, pediatric emergency visits for diphenhydramine misuse rose 27%. Kids accidentally overdosed on liquid versions, thinking it was candy. The UK banned over-the-counter promethazine for minors in 2022. The FDA is considering similar rules.Who Should Avoid Them Completely
If you fall into any of these groups, skip first-generation antihistamines:- People over 65
- Those with glaucoma, enlarged prostate, or urinary retention
- Anyone taking other sedatives, opioids, or alcohol
- People who drive, operate machinery, or work in safety-sensitive jobs
- Those with a history of cognitive decline or dementia
- Anyone using them regularly for sleep or allergies
What to Use Instead
Second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) are the modern standard. They barely enter the brain. Brain concentrations stay below 1 ng/mL-even at full doses. That means no drowsiness, no brain fog, no next-day hangover. They’re not perfect. Some people still get mild tiredness with cetirizine. But overall, they’re safer, longer-lasting (12-24 hours), and don’t interfere with cognition. For allergies, they’re just as effective. For motion sickness? Less so. But for most people, the trade-off is worth it. For sleep, try melatonin or behavioral changes. For nausea, ginger or prescription options like ondansetron. There are alternatives for every use case.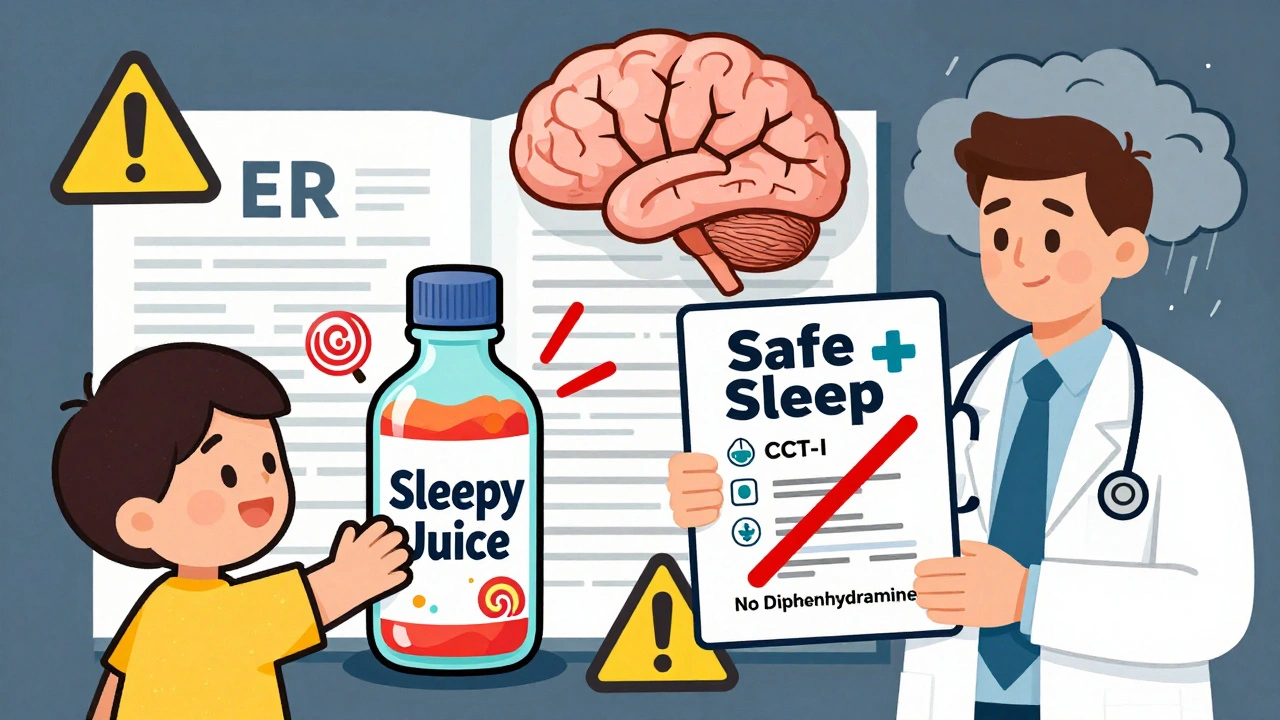
How to Use Them Safely (If You Must)
If you’re using one of these drugs-say, for a short trip or one bad night of allergies-follow these rules:- Take it only at bedtime. Never during the day.
- Start with the lowest dose: 12.5 mg for diphenhydramine.
- Avoid alcohol completely. It doubles the sedative effect.
- Wait at least 8 hours before driving or operating machinery-even if you feel awake.
- Don’t use it for more than 3-5 days in a row.
- Check all OTC meds. Many cold and sleep aids contain hidden diphenhydramine.
The Future Is Clearer
Pharmaceutical companies are working on “third-generation” antihistamines designed to stay out of the brain. Two candidates, EB-029 and DP-118, are in clinical trials with 80% less brain penetration than diphenhydramine. They promise the same allergy relief without the fog. The FDA is also tightening labeling. New packaging must now warn about next-day impairment. That’s progress. But until these new drugs hit the market, the choice is simple: if you need to think clearly, stay awake, or protect your long-term brain health-choose something else.It’s Not About Being Scared. It’s About Being Smart.
First-generation antihistamines aren’t evil. They saved lives in the 1940s. They still help in specific situations. But they’re not the safe, harmless pills many think they are. Their side effects aren’t rare. They’re predictable. And they’re dangerous-especially when used without awareness. You don’t need to avoid them forever. But you do need to know what you’re really signing up for. If you’re using them because they’re cheap or convenient, ask yourself: is a few hours of relief worth hours of brain fog-or worse?Are first-generation antihistamines safe for occasional use?
Occasional use-like one dose for a bad allergy night or a long car trip-is generally low-risk for healthy adults under 65. But even then, avoid driving, operating machinery, or making important decisions for at least 8 hours after taking them. The risk isn’t in the single dose-it’s in the habit. Using them regularly, even once a week, increases anticholinergic burden over time.
Why do some people get drowsy and others don’t?
It comes down to genetics. About 7% of people are CYP2D6 poor metabolizers, meaning their liver breaks down these drugs very slowly. That leads to higher brain concentrations and stronger side effects. Others may have more sensitive H1 receptors in the brain. Age, weight, and liver health also play a role. There’s no way to predict your reaction before trying it-so always start low and go slow.
Can I take first-generation antihistamines with other medications?
Avoid combining them with alcohol, opioids, benzodiazepines, sleep aids, or certain antidepressants. These all boost sedation. They’re also metabolized by the same liver enzymes (CYP2D6 and CYP3A4) as statins, blood pressure drugs, and some antibiotics. Mixing them can lead to dangerous buildup. Always check with a pharmacist before combining any OTC meds.
Do second-generation antihistamines cause any side effects?
Yes, but they’re much milder. Some people report mild headaches, dry mouth, or fatigue with cetirizine-but it’s rare and usually goes away. They don’t cause urinary retention, blurred vision, or cognitive decline. For most people, the side effect profile is far better than the trade-offs of first-generation drugs.
Is it safe to use diphenhydramine as a sleep aid long-term?
No. While it helps you fall asleep faster, it disrupts deep and REM sleep stages. Over time, your body builds tolerance, requiring higher doses. Long-term use is linked to increased dementia risk, especially in older adults. Better options include melatonin, cognitive behavioral therapy for insomnia (CBT-I), or addressing underlying causes like sleep apnea or anxiety.
What should I do if I’ve been taking these for months?
Don’t stop abruptly. Talk to your doctor. They can help you switch to a safer alternative like loratadine for allergies or melatonin for sleep. If you’ve been using them for insomnia, consider CBT-I-it’s more effective long-term than any pill. And if you’re over 65, this is especially urgent. Your brain has already been exposed to more anticholinergic burden than most realize.


Deborah Jacobs
Been taking Benadryl for years like it was candy. Woke up one morning and couldn’t remember my kid’s birthday. That’s when I knew something was wrong. Now I use Zyrtec. No fog. No guilt. Just clean, quiet relief. My brain thanks me.
Stephanie Fiero
ok so i just took 2 benadryl last night bc i had a rash and woke up at 4pm like i got hit by a bus?? like what even is this?? why is this even legal?? someone please explain to me why my pharmacy sells this like it’s gummy vitamins??
sean whitfield
They don’t want you to know this but the FDA is in bed with Big Pharma. Why else would they let these brain-rot pills sit on shelves next to aspirin? It’s not about safety. It’s about profit. You think they care if you forget your own name? No. They just want your money. And your silence.
Marvin Gordon
My grandma used to take this for sleep. I didn’t realize until she started forgetting my name that it was the meds. Took her off it. Switched to melatonin. Her memory came back. Slowly. But it came back. Don’t wait until it’s too late. Your brain doesn’t get a do-over.
William Chin
It is imperative that the general populace be made aware of the neurotoxic potential inherent in the chronic utilization of first-generation antihistaminergic agents. The pharmacokinetic profile of diphenhydramine, in particular, demonstrates an alarming propensity for cumulative anticholinergic burden, which has been empirically correlated with accelerated neurodegeneration in longitudinal cohort studies. One must exercise extreme prudence.
Lucy Kavanagh
They’re doing this on purpose. You think it’s an accident that these drugs make you drowsy? No. They want you sluggish. Less productive. Less likely to question the system. That’s why they’re in every cold medicine, every sleep aid, every cheap allergy pill. It’s control. And it’s working.
Chris Brown
People who use these drugs casually are not just irresponsible-they are morally negligent. You think your ‘occasional’ use is harmless? It’s not. You’re not just hurting yourself. You’re endangering others on the road, in the workplace, in your own home. Wake up. This isn’t a lifestyle choice. It’s a public health failure.
Michael Dioso
Yeah sure, Zyrtec’s fine. But have you ever tried it? Half the time it does jack. And don’t get me started on how expensive it is. Meanwhile, Benadryl knocks me out like a punch to the face-and I don’t care. If I gotta be a zombie for a day to stop sneezing, so be it. I’ll take the fog over a runny nose any day.
Krishan Patel
It is written in the Vedas that the mind must remain pure, unclouded by artificial substances. The modern man, intoxicated by convenience, forgets that the body is a temple. To poison it with diphenhydramine is to invite chaos into the soul. The West has lost its way. We must return to nature, to truth, to clarity.
Carole Nkosi
They told us these pills were safe. They lied. They always lie. I used to take them every night for sleep. Now I can’t remember my own childhood. They took it. They took my memories. And they sold it to you for five bucks. Don’t be next.
Jennifer Patrician
Benadryl is a gateway drug. First it’s for allergies. Then it’s for sleep. Then it’s for anxiety. Then you’re popping them with vodka because you can’t feel anything anymore. They’re not pills. They’re emotional anesthetics. And they’re turning us into ghosts.
Manish Shankar
Thank you for this comprehensive and scientifically grounded exposition. The empirical evidence presented regarding anticholinergic burden and its association with long-term cognitive decline is both compelling and deeply concerning. It is my sincere hope that regulatory bodies will enforce stricter labeling requirements and public education campaigns to mitigate further harm.
luke newton
You think you’re the first person to figure this out? Everyone knows this. Everyone. But nobody wants to admit it because then they’d have to stop using the thing that makes them feel ‘normal.’ You’re not special. You’re just the latest one pretending to be awake.