When you’re trying to manage type 2 diabetes and lose weight at the same time, most medications make it harder - not easier. Insulin and sulfonylureas often lead to weight gain. Metformin helps a little with weight but rarely delivers major results. That’s where GLP-1 receptor agonists change the game. These aren’t just diabetes drugs anymore. They’re turning into powerful tools for lasting weight loss, with real data backing up claims of 10%, 15%, even 20% body weight reduction.
How GLP-1 Receptor Agonists Actually Work
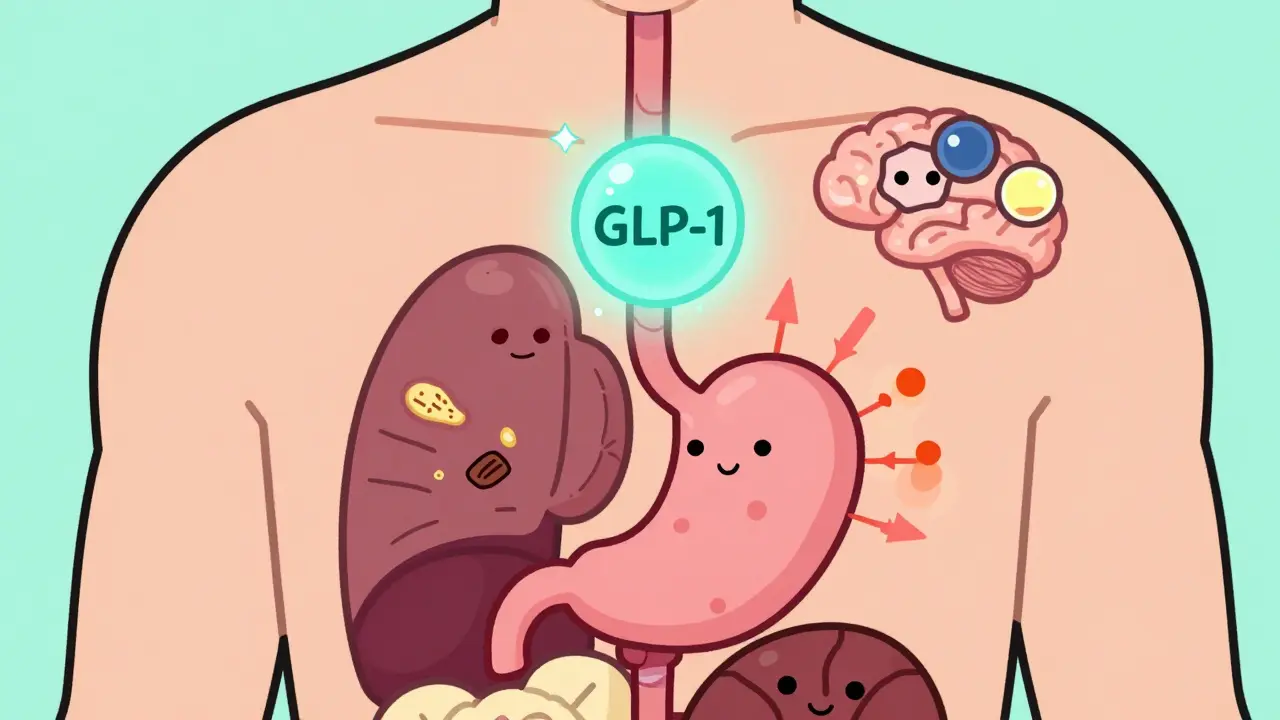
GLP-1 receptor agonists mimic a hormone your body already makes - glucagon-like peptide-1. This hormone is released after you eat, signaling your pancreas to release insulin and telling your brain you’re full. But in people with type 2 diabetes or obesity, this system doesn’t work well. GLP-1 agonists step in and boost what’s missing.
They do three big things:
- Slow down how fast food leaves your stomach - by 15% to 30%. That means sugar enters your bloodstream slowly, avoiding spikes.
- Stimulate your pancreas to release insulin only when blood sugar is high. This reduces the risk of low blood sugar compared to other diabetes drugs.
- Act on your brain’s appetite center. They turn down hunger signals and boost fullness signals, making you feel satisfied with less food.
It’s not magic. It’s biology. Studies show these drugs reduce appetite by 30% to 40% in clinical trials. That’s why people stop craving junk food. One user on a patient forum said, “I no longer crave sugar - it’s like my brain rewired itself.” That’s not anecdotal. Brain imaging studies confirm GLP-1 agonists reduce activity in areas tied to food reward.
Weight Loss Numbers You Can Trust
Not all GLP-1 drugs are the same. The weight loss you get depends on the drug and the dose.
Here’s what real trials show:
| Drug (Brand) | Dose | Average Weight Loss | A1C Reduction |
|---|---|---|---|
| Semaglutide (Wegovy) | 2.4 mg weekly | 14.9% | 1.8% |
| Tirzepatide (Zepbound) | 15 mg weekly | 20.9% | 2.4% |
| Liraglutide (Saxenda) | 3.0 mg daily | 6.4% | 1.1% |
| Dulaglutide (Trulicity) | 1.5 mg weekly | 4.5% | 1.5% |
| Exenatide (Byetta) | 10 mcg twice daily | 2.5% | 0.9% |
These aren’t small numbers. Losing 15% of your body weight is what used to require bariatric surgery. The STEP 8 trial showed semaglutide led to 15.8% weight loss over 68 weeks - more than double what liraglutide achieved. Tirzepatide, a newer dual-acting drug that also targets GIP, pushed past 20% in some trials. That’s the highest weight loss ever seen with a non-surgical treatment.
Why GLP-1 Drugs Beat Other Diabetes Medications
Let’s compare GLP-1 agonists to other common diabetes treatments:
- Insulin: Causes weight gain - often 4 to 10 kg. It lowers blood sugar but makes it harder to lose fat.
- Sulfonylureas (like glimepiride): Also cause weight gain. They force the pancreas to pump out insulin, even when it’s not needed.
- DPP-4 inhibitors (like sitagliptin): Mild A1C reduction (0.5-1.0%), no weight change. They just extend the life of your body’s own GLP-1 - not strong enough to make a big difference.
- SGLT2 inhibitors (like empagliflozin): Lose 2-5 kg. They make your kidneys dump sugar in urine. Good for heart and kidneys, but less effective for appetite control.
GLP-1 agonists are the only class that consistently delivers both strong A1C drops and major weight loss. That’s why the American Diabetes Association now recommends them as first-line for people with type 2 diabetes who are overweight - even before metformin in some cases.

The Catch: Side Effects and Challenges
These drugs aren’t easy to start. Most people get nausea, especially in the first few weeks. Up to 50% of users report stomach issues during dose escalation. Vomiting happens in 5-10%, and diarrhea in 20-25%. That’s why doctors start low and go slow.
For semaglutide (Wegovy), the standard titration looks like this:
- Weeks 1-4: 0.25 mg once a week
- Weeks 5-8: 0.5 mg
- Weeks 9-12: 1.0 mg
- Weeks 13-16: 1.7 mg
- Week 17+: 2.4 mg (maintenance)
You don’t feel the full effect until you hit the top dose - which takes about 5 months. Many people give up before then because of nausea. But if you stick with it, side effects usually fade. Experts recommend taking the shot at bedtime, avoiding fatty meals during titration, and using over-the-counter anti-nausea meds like dimenhydrinate if needed.
Another hurdle? Cost. Without insurance, these drugs cost $800 to $1,200 a month in the U.S. Even with insurance, prior authorization is common. Medicare covers about 62% of prescriptions - but only after you’ve tried other weight loss methods first.
And then there’s the needle factor. Some people hate injections. But most get used to it. A 2022 survey found 85% of patients self-administer successfully after two or three training sessions. Needle anxiety drops fast once you realize how thin the needle is - thinner than most insulin needles.
What Happens When You Stop Taking Them?
This is the big question no one talks about enough. If you stop taking a GLP-1 agonist, you’ll likely regain weight. Studies show people regain 50% to 70% of lost weight within a year after stopping.
That doesn’t mean the drug failed. It means the condition - obesity or insulin resistance - is still there. These drugs don’t cure anything. They manage it. Think of them like blood pressure pills. You don’t stop taking them after your pressure normalizes. You keep going.
Some doctors are now exploring “maintenance dosing” - keeping patients on a lower dose long-term. Others suggest combining them with lifestyle changes so the body adapts to a new weight set point. The goal isn’t just to lose weight - it’s to make the new weight stick.

New Frontiers: Beyond Weight and Diabetes
Researchers are now testing GLP-1 drugs for conditions no one expected:
- Non-alcoholic fatty liver disease (NAFLD): Semaglutide reduced liver fat by 52% in a 2024 Lancet trial - far better than placebo.
- Heart failure: The STEP-HFpEF trial showed semaglutide improved walking distance and reduced breathlessness in obese patients with heart failure.
- Alzheimer’s prevention: Novo Nordisk is testing oral semaglutide in early-stage Alzheimer’s patients. Early data suggests it may slow brain changes linked to the disease.
These aren’t side effects. They’re benefits tied to the same mechanism: reducing inflammation, improving insulin sensitivity, and protecting nerve cells.
Who Should Consider GLP-1 Agonists?
You might be a good candidate if:
- You have type 2 diabetes and are overweight or obese (BMI ≥27)
- You’ve tried diet and exercise but haven’t lost significant weight
- You’re willing to commit to long-term treatment
- You can manage the cost or have insurance coverage
- You’re okay with weekly injections
They’re not for everyone. People with a personal or family history of medullary thyroid cancer or multiple endocrine neoplasia type 2 should avoid them. Pregnant women shouldn’t use them. And they’re not a quick fix for people who just want to lose 5 pounds.
The real power of these drugs is for people with metabolic syndrome - high blood sugar, high blood pressure, belly fat, and high cholesterol. For them, GLP-1 agonists don’t just help with weight. They lower the risk of heart attack, stroke, and kidney disease.
The Future Is Here - And It’s Growing
The global market for GLP-1 drugs hit $23.5 billion in 2022 and is expected to hit $48 billion by 2028. Semaglutide alone made $10.8 billion for Novo Nordisk in 2023. Demand is so high that Wegovy has been on FDA shortage lists since early 2022.
Oral versions are coming. Novo Nordisk has an oral semaglutide pill approved for diabetes (Rybelsus), and trials for an oral weight-loss version are underway. That could change everything - no more needles, easier access.
And then there’s tirzepatide - the dual agonist. It’s already approved for both diabetes and obesity under the names Mounjaro and Zepbound. It’s stronger than semaglutide in head-to-head trials. It’s the new gold standard.
These drugs aren’t just changing how we treat diabetes. They’re changing how we think about obesity. It’s not a lack of willpower. It’s a hormonal imbalance. And now, we have medicines that fix it.
How long does it take to see weight loss on GLP-1 agonists?
Most people start seeing weight loss within 4 to 8 weeks, but the biggest drops happen after reaching the full dose - usually around 16 to 20 weeks. The STEP trials showed the most significant results at 68 weeks. Patience and consistency matter more than speed.
Can I take GLP-1 agonists if I don’t have diabetes?
Yes. Wegovy and Zepbound are FDA-approved specifically for chronic weight management in adults with a BMI of 30 or higher, or 27 or higher with at least one weight-related condition like high blood pressure or sleep apnea. You don’t need to have diabetes to qualify.
Are GLP-1 agonists safe for long-term use?
Current data shows they’re safe for long-term use. The LEADER trial followed patients on liraglutide for over 5 years and found no increase in serious side effects. In fact, they reduced heart attacks and strokes in high-risk patients. Ongoing studies are tracking users for 10+ years. So far, the benefits outweigh the risks for most people.
Why are these drugs so expensive?
They’re biologics - complex proteins made using living cells. Manufacturing them is expensive. Demand has exploded, and supply hasn’t kept up. Drugmakers are investing in new production facilities, but it takes years. Insurance coverage is improving, but out-of-pocket costs remain high without coverage.
Do I need to diet and exercise while on GLP-1 agonists?
Yes. These drugs work best when paired with healthy eating and physical activity. They reduce hunger and help you stick to a plan, but they don’t replace good habits. People who combine them with lifestyle changes lose more weight and keep it off longer.
Is there a pill version of GLP-1 agonists?
Yes - Rybelsus is an oral semaglutide approved for type 2 diabetes. It’s taken daily on an empty stomach. An oral version for weight loss is in late-stage trials and could be available by 2027. That will make these drugs much more accessible.

Darren McGuff
Let’s be real - these drugs aren’t a miracle. They’re a Band-Aid on a broken metabolic system. I’ve seen patients lose 20% of their body weight on tirzepatide, then gain it all back within months of stopping. The real issue? We treat obesity like a cosmetic problem, not a chronic disease. We give people a pill and tell them to ‘stay consistent,’ but we don’t fix the food environment, the stress, the sleep deprivation, or the systemic neglect of mental health. This isn’t medicine. It’s pharmaceutical capitalism dressed up as science.
Lindsey Wellmann
OMG I started semaglutide last month and I literally haven’t craved pizza since 😭 I used to eat an entire large pie by myself on Friday nights… now I just stare at it like it’s a foreign object. My husband thinks I’ve been replaced by a robot. Also, nausea hit hard week 2 but I took it at bedtime and now I’m fine. 11 lbs down!! 🎉
Angela Stanton
Let’s analyze the data: The STEP 8 trial’s 15.8% weight loss with semaglutide was statistically significant (p<0.001), but the effect size was confounded by selection bias - participants were highly motivated, had baseline BMI >35, and received weekly coaching. Real-world adherence? 62% drop-off by week 20. Also, the 20.9% loss with tirzepatide? That’s from SURMOUNT-1, which excluded anyone with prior GLP-1 exposure. So yes, the numbers are impressive - but they’re not generalizable. This is precision medicine, not population health.
Diana Stoyanova
Y’all are missing the point. This isn’t just about weight loss - it’s about dignity. I spent 15 years being told I just needed to ‘eat less and move more.’ I did. I ran marathons. I counted every calorie. I was exhausted. Then I got on semaglutide. Suddenly, I wasn’t fighting my own biology every second of the day. I could breathe. I could think. I could be present with my kids. These drugs don’t make you lazy - they give you back your energy. And if you think that’s not worth $1,000 a month, you’ve never been hungry all the time because your brain won’t let you stop eating. This isn’t vanity. It’s survival.
Ashley Kronenwetter
While the clinical data supporting GLP-1 receptor agonists is compelling, it is imperative to acknowledge the ethical implications of their commercialization. The current pricing structure, coupled with insurance gatekeeping, creates a two-tiered healthcare system wherein only the affluent can access life-altering therapeutics. This raises fundamental questions regarding distributive justice in public health policy. We must advocate for equitable access, not merely expand prescription volume.
Heather Wilson
So let me get this straight - you’re telling me that people who can’t control their eating habits are now just going to inject a drug and call it a day? No accountability. No discipline. No personal responsibility. This is the end of Western civilization. We used to fight through hunger. Now we just pop a needle and pretend biology doesn’t exist. And don’t get me started on the fact that these drugs are being marketed as ‘weight loss’ when they’re clearly designed for people with metabolic disease. You’re normalizing addiction to pharmaceuticals for aesthetic purposes. Disgusting.
Drew Pearlman
I know it sounds crazy, but I’ve been on liraglutide for 8 months and I actually feel like myself again. Not the ‘fat me’ - the me I was before 2018. I’m sleeping better. My knees don’t hurt. I went hiking with my niece last weekend and didn’t need to stop three times. I’m not saying this is perfect, but it’s the first time in my life I’ve felt like my body isn’t working against me. If you’re scared of needles, start with the lowest dose. If you’re scared of cost, talk to your pharmacist - there are patient assistance programs. You don’t have to do this alone.
Meghan Hammack
Hey, if you’re thinking about this - you’ve already won half the battle. Just start slow. Don’t compare yourself to the 20% losers on TikTok. Your journey is yours. Nausea? Totally normal. Take it at night. Skip the greasy food. Drink ginger tea. You’ve got this. And if you feel like quitting? That’s okay. Try again next month. This isn’t a race. It’s a reset.
Kiruthiga Udayakumar
In India, we don’t have access to these drugs - not even for diabetics. But we have turmeric, neem, and centuries of Ayurvedic wisdom. Why are we chasing Western pharmaceuticals when our ancestors knew how to balance blood sugar with diet and herbs? This is cultural imperialism disguised as medical progress. We need solutions that fit our realities, not expensive injections that only the rich can afford.
Maggie Noe
It’s fascinating how we’ve turned biology into a moral narrative. People who use these drugs are either ‘heroes’ or ‘cheaters.’ But what if the truth is simpler? Your body has a set point. These drugs nudge it. That’s it. No judgment. No virtue. Just physiology. We’re not broken. We’re just… regulated differently. Maybe the real failure isn’t in our willpower - it’s in our belief that we should be able to control everything with discipline alone.
Catherine Scutt
These drugs are a scam. You’re not losing weight - you’re just being chemically sedated into not eating. And when you stop? You gain back everything plus interest. The pharmaceutical industry made $10 billion off this. You think they care about your health? They care about your subscription. Don’t be fooled.
Alicia Hasö
If you’re reading this and wondering whether to try it - I want you to know: you deserve to feel good in your body. Not because you’re ‘thin,’ but because you’re alive. These drugs aren’t magic, but they’re tools. And tools don’t make you weak - they make your work easier. Pair them with movement you enjoy. Eat food you love. Rest when you need to. This isn’t about perfection. It’s about peace. You’re not behind. You’re exactly where you need to be to begin.
Chris Kauwe
Let’s deconstruct the hegemony of the metabolic model. The GLP-1 paradigm reinforces a biomedical reductionism that pathologizes fatness while ignoring structural determinants: food deserts, wage stagnation, chronic stress, and racialized healthcare disparities. The fact that we celebrate a $1,200/month injection as a ‘solution’ reveals the rot of late-stage capitalism in medicine. We don’t need more drugs - we need food sovereignty, universal healthcare, and the dismantling of weight stigma as a social construct. This isn’t progress. It’s commodified oppression.
Ian Long
Look - I get the fear. I was scared of needles too. I thought I’d be ‘that guy’ injecting himself at the office. But I did it. Took me three tries to get the hang of it. Now I do it while watching Netflix. The nausea? Lasted two weeks. The weight loss? Real. The confidence? Better than any weight loss program I’ve ever tried. I’m not saying it’s perfect. But it’s the first thing that actually worked. And if you’re on the fence - just talk to your doctor. No judgment. Just ask.
Elisha Muwanga
These drugs are a luxury for the privileged. Meanwhile, my cousin in rural Alabama can’t even get a basic diabetes test without driving 90 miles. We’re celebrating a $1,000/month injection while millions can’t afford insulin. This isn’t medicine - it’s a distraction. We need to fix the system, not sell Band-Aids to the rich.