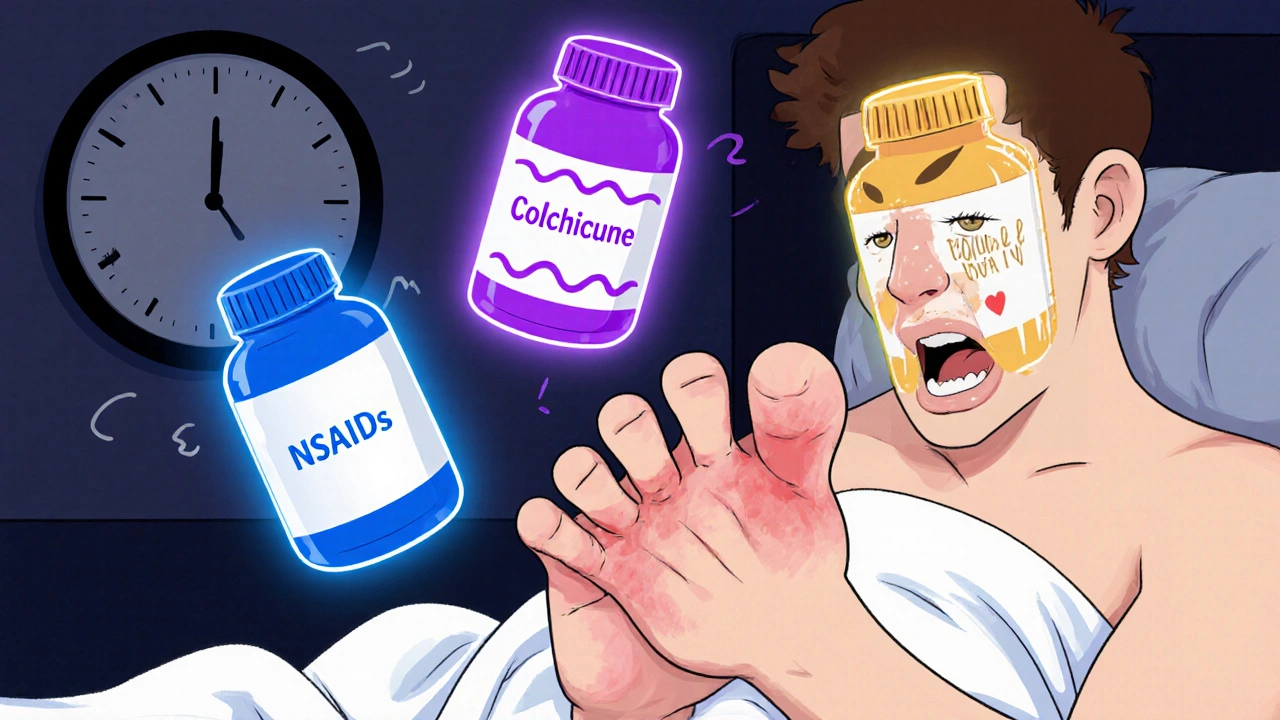
When a gout flare hits, it doesn’t ask for permission. One minute you’re fine, the next, your big toe feels like it’s been crushed under a boot. The pain is sharp, swelling rolls in fast, and even a sheet touching your skin feels unbearable. If you’ve been through this, you know waiting it out isn’t an option. You need relief - fast. And that’s where colchicine, NSAIDs, and steroids come in. These are the three main drugs doctors reach for when gout flares up. But which one’s right for you? It’s not about which is strongest. It’s about which fits your body.
What Happens During a Gout Flare?
Gout isn’t just bad joint pain. It’s inflammation caused by uric acid crystals forming in your joints. When these sharp little crystals trigger your immune system, your body goes into overdrive. Blood rushes to the area, white blood cells swarm in, and everything swells, turns red, and screams. The first flare often hits the big toe, but ankles, knees, wrists, and fingers aren’t safe either. These flares don’t come out of nowhere. They’re usually tied to diet, dehydration, alcohol, or sudden changes in uric acid levels. But once the pain starts, the clock starts ticking. Treatment needs to begin within 24 hours - ideally sooner - to stop the inflammation from digging in deep.
NSAIDs: The Go-To for Most People
Nonsteroidal anti-inflammatory drugs like naproxen, ibuprofen, and indomethacin are the most common first choice for gout flares. They work by blocking the enzymes that cause inflammation and pain. For gout, you need high doses. That means 500 mg of naproxen twice a day, 800 mg of ibuprofen three times a day, or 50 mg of indomethacin three times a day - for about 3 to 5 days. Only three NSAIDs have FDA approval specifically for gout: indomethacin, naproxen, and sulindac. But in practice, doctors use any NSAID at full anti-inflammatory doses.
Here’s the catch: NSAIDs are tough on your gut, kidneys, and heart. If you’ve got stomach ulcers, high blood pressure, kidney disease, or take blood thinners, NSAIDs can make things worse. That’s a big deal because most people with gout are over 50 and already managing other conditions. Studies show that NSAID side effects are especially common in older adults. One study found naproxen caused fewer side effects than low-dose colchicine, even though both worked just as well at reducing pain over seven days. But if your stomach is sensitive or your kidneys are weak, NSAIDs aren’t worth the risk.
Colchicine: Low Doses, Big Results
Colchicine used to mean taking a whole handful of pills over six hours - and then spending the next day in the bathroom. That’s changed. New research shows you get the same pain relief with just 1.8 mg total - taken as 1.2 mg at the first sign of pain, then 0.6 mg an hour later. That’s a big drop from the old 4.8 mg dose. The result? Less diarrhea, less nausea, and fewer people quitting because they couldn’t handle the side effects.
But colchicine has its own dangers. It’s got a narrow therapeutic window. That means the difference between a helpful dose and a toxic one is small. If you have kidney or liver problems, your body can’t clear it well. That can lead to muscle damage, nerve issues, or even life-threatening reactions like rhabdomyolysis or disseminated intravascular coagulation. It’s also risky if you’re on statins or certain antibiotics. Your doctor will check your meds and your kidney function before prescribing it. It’s not the easiest drug to use, but when it works, it works fast - and it’s cheap.
Steroids: The Quiet Contender
Steroids - like prednisone - are often overlooked, but they’re one of the most effective tools for gout. Oral prednisone is usually started at 40-60 mg a day, then slowly lowered over 10-14 days. This tapering is key. Stopping too fast can cause your gout to flare again. Intra-articular injections - a shot directly into the inflamed joint - are even better for single-joint flares. No stomach upset. No kidney strain. Just targeted relief.
Why aren’t steroids used more? Some doctors worry about blood sugar spikes in diabetics, or the idea that steroids are “strong” drugs. But the truth is, a short 10-day course is safe for most people. In fact, a major 2017 meta-analysis of six trials found steroids reduced pain just as well as NSAIDs - and had fewer serious side effects. Medical experts now say corticosteroids are equally or even more effective than NSAIDs and colchicine, with much less risk of toxicity. For older patients, those with kidney disease, or anyone who can’t take NSAIDs or colchicine, steroids are often the best choice. They’re also inexpensive and widely available.
Which One Should You Choose?
There’s no single answer. The right drug depends on your health, your meds, and your history.
- If you’re young, healthy, and have no stomach or kidney issues - NSAIDs are fine. Naproxen is often preferred over ibuprofen because it’s easier on the stomach.
- If you’ve had bad side effects from NSAIDs, or you’re on blood thinners - colchicine at low dose might work. But only if your kidneys are okay and you’re not on conflicting meds.
- If you’re over 60, have high blood pressure, diabetes, or kidney disease - steroids (oral or injected) are often the safest and most effective option.
- If only one joint is flaring - ask about a steroid injection. It’s fast, local, and avoids system-wide side effects.
Some people need more than one drug. If one isn’t enough, your doctor might combine steroids with colchicine, or NSAIDs with colchicine. This isn’t common, but it’s done when flares are severe or stubborn.
What About Long-Term?
Treating the flare is only half the battle. If you’re on uric acid-lowering drugs like allopurinol or febuxostat, you’re still at risk for flares - especially in the first few months. That’s why guidelines say you need to take preventive meds for at least three months after your uric acid drops below 6 mg/dL. If you’ve had tophi (those lumpy deposits under the skin), you need six months of protection. The best options for prevention? Low-dose colchicine, low-dose NSAIDs, or low-dose steroids. The goal isn’t to avoid flares forever - it’s to give your body time to clear out old crystals without triggering new ones.
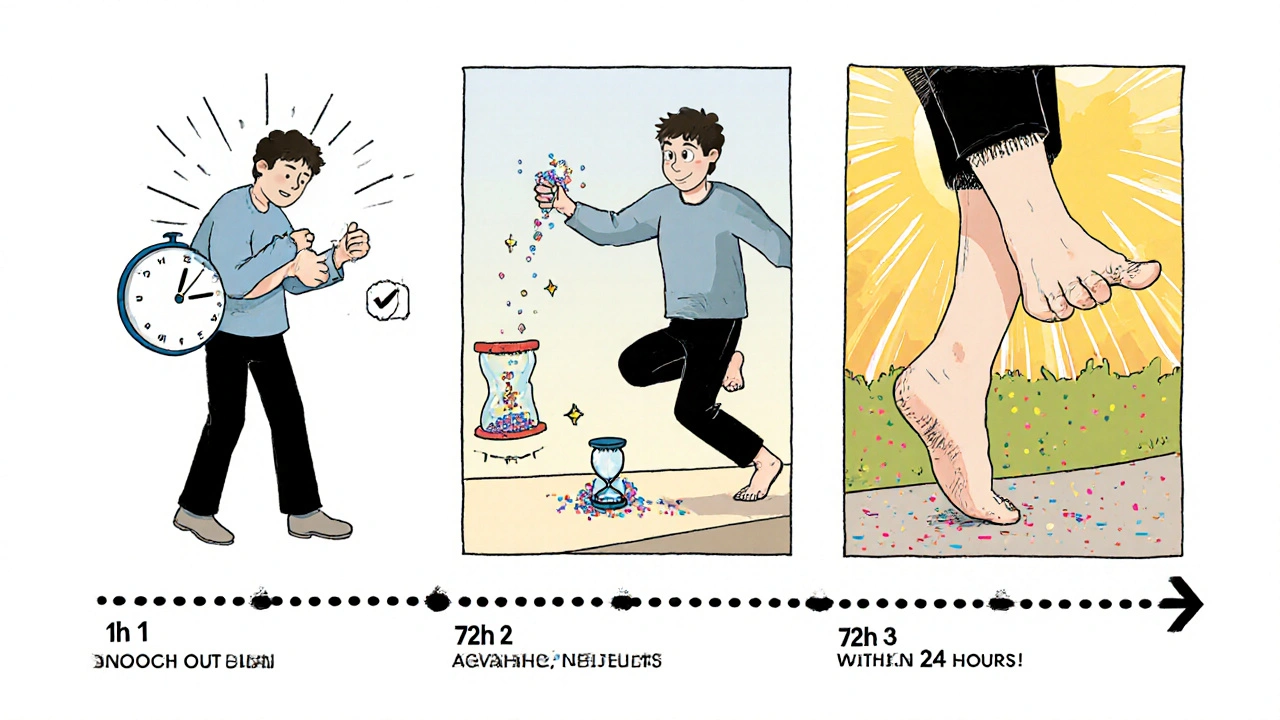
Timing Is Everything
Here’s the most important thing: don’t wait. The sooner you start treatment after pain begins, the better it works. One rheumatologist says to start within 24 seconds of pain - meaning, don’t delay. If you wait 48 hours, the inflammation is already locked in. You’ll need higher doses, longer treatment, and still might not get full relief. Keep your meds on hand. If you’ve had flares before, know what works. Have your prescription ready. Don’t wait for your doctor’s appointment. Get started now.
What You Can Do Today
- If you’re having a flare, start your meds within 24 hours.
- If you’re unsure which drug to use, call your doctor - don’t guess.
- If you’re on allopurinol or febuxostat, make sure you’re also on a preventive dose of colchicine or NSAIDs.
- If you’re over 60 or have kidney problems, ask about steroids instead of NSAIDs.
- If only one joint hurts, ask if an injection is an option.
Gout flares are brutal, but they’re manageable. You don’t need to suffer through them. The right drug, at the right time, can get you back on your feet in days - not weeks.
Can I take NSAIDs if I have high blood pressure?
NSAIDs can raise blood pressure and interfere with blood pressure medications. If you have high blood pressure, especially if it’s not well controlled, NSAIDs are risky. Steroids or low-dose colchicine are safer options. Always check with your doctor before starting any new pain reliever.
Is colchicine safe for people with kidney disease?
Colchicine is cleared by the kidneys. If you have moderate to severe kidney disease, your body can’t remove it properly, which increases the risk of serious toxicity. Doses must be lowered significantly - or avoided entirely. Your doctor will check your kidney function with a blood test before prescribing it.
Why do steroids need to be tapered?
Stopping steroids suddenly can cause your gout to flare again - sometimes worse than before. Tapering slowly over 10-14 days helps your body adjust and prevents rebound inflammation. Even if you feel better after a few days, finish the full taper as prescribed.
Can I use steroids if I have diabetes?
Yes - but you need to monitor your blood sugar closely. Steroids can cause spikes in glucose levels, even with short courses. If you have diabetes, your doctor may adjust your insulin or oral meds during treatment. It’s manageable with careful monitoring.
What’s the fastest way to relieve gout pain?
For a single joint flare, a steroid injection into the joint is the fastest and most targeted relief - often working within hours. If that’s not possible, starting a low-dose colchicine regimen or a high-dose NSAID within 24 hours of pain onset gives the best chance for quick improvement.
Do I need to take medication for gout forever?
No - you don’t need to take flare meds forever. But if you’re on long-term uric acid-lowering drugs like allopurinol, you’ll need preventive meds (like low-dose colchicine) for at least three to six months after your uric acid levels drop below target. This prevents new flares while your body clears old crystals.
Final Thoughts
Gout flares are painful, but they’re not a life sentence. The key isn’t finding the “best” drug - it’s finding the right one for your body. NSAIDs work well if your stomach and kidneys are healthy. Colchicine is effective but needs careful dosing. Steroids offer strong relief with fewer risks for many older or high-risk patients. The best choice isn’t the one you read about online - it’s the one your doctor recommends after looking at your full health picture. And don’t wait. Start treatment early. That’s the real game-changer.

Robert Merril
NSAIDs my ass i took ibuprofen for a gout flare and it did jack shit while my buddy took colchicine and was walking like a normal human by noon
Noel Molina Mattinez
steroids are the real answer no one talks about them because they scared of the word steroid like its crack cocaine
Roberta Colombin
Thank you for this clear and thoughtful breakdown. Many people feel alone with gout, and knowing there are safe, effective options can bring real peace of mind. Always consult your doctor, but please don't suffer in silence. You deserve relief.
Dave Feland
It's fascinating how the medical establishment still clings to NSAIDs as first-line despite overwhelming evidence of their cardiovascular and renal toxicity. The real agenda here? Pharmaceutical lobbying. Colchicine is cheap, steroids are older than penicillin, and neither has a multi-billion dollar marketing campaign behind it. The system is rigged to keep you dependent on expensive, dangerous drugs.
mike tallent
This is gold 🙌 I had a flare last month and my doc pushed NSAIDs but my stomach was screaming. I asked about steroids and she gave me a 5-day prednisone taper. Game changer. No more bathroom trips. Just pain gone. 💪
John Wayne
Colchicine is overrated. I've had three flares. NSAIDs worked every time. Steroids? That's just chemical suppression. You're not fixing the root cause. You're just silencing the messenger. Eventually the crystals come back louder.
Julie Roe
I just want to say to anyone reading this who’s been told to just ‘live with it’ or ‘it’s just gout’ - you’re not crazy. This pain is real and it’s brutal. And the fact that you’re researching this means you’re already doing the right thing. Don’t let anyone make you feel like you’re overreacting. You’re not. Your body is screaming and it deserves to be heard. And yes, steroids are okay. They’re not magic, they’re medicine. And sometimes medicine is gentle.
jalyssa chea
colchicine gave me diarrhea so bad i had to call 911 and now im scared to take anything even my doc says its fine but i dont trust him anymore
Gary Lam
lol i thought steroids were for bodybuilders until i got my first gout flare. now i’m like hey prednisone you’re my new best friend 😎
Peter Stephen .O
Man I used to think gout was just a rich man's disease until I saw my uncle's toe swell up like a balloon and he's a janitor who eats beans and rice. The truth? It's not about what you eat - it's about how your body handles uric acid. And honestly? If you're over 50 and your kidneys are slowing down? Steroids aren't scary - they're smart. Don't let fear stop you from feeling human again.
Andrew Cairney
They don't want you to know this but steroids are used in the military to suppress inflammation after combat injuries - and they're given in high doses. So why are we scared of them for gout? Coincidence? I think not. Big Pharma hates steroids because they're cheap, effective, and can't be patented. This is all about profit. Your doctor knows. I know. You know. We're just not supposed to talk about it. 🕵️♂️