Dental Anesthesia Effectiveness Calculator
| Agent | Onset (min) | Duration (min) |
|---|---|---|
| Lidocaine | 2–4 | 60–120 |
| Articaine | 1–2 | 80–180 |
| Mepivacaine | 3–5 | 45–90 |
Estimated Pain Reduction
Your estimated pain reduction: 0%
Based on clinical studies showing 78% average pain reduction with proper technique.
Quick Takeaways
- Local anesthesia blocks pain signals at the source, reducing discomfort in >90% of routine dental work.
- Lidocaine and articaine are the most widely used agents; articaine offers a faster onset and slightly longer duration.
- Technique matters - a well‑placed inferior alveolar nerve block can halve perceived pain scores compared with a superficial injection.
- Patient anxiety, inflammation, and the presence of vasoconstrictors influence how well the anesthetic works.
- Side effects are rare, and proper dosing keeps the procedure safe for adults and children alike.
When you sit in a dentist’s chair, the fear of pain is often the biggest hurdle. The promise that the needle will “numb” the area is backed by decades of research, but how good is that promise really? This article breaks down the science, looks at the numbers from recent clinical trials, and gives you practical tips to make sure you get the most pain‑free experience possible.
What Is Local Anesthesia?
Local Anesthesia is a medication that temporarily blocks nerve conduction in a small, targeted region of the body. By preventing the nerves from transmitting pain signals to the brain, the dentist can perform drilling, extractions, or fillings without you feeling the usual sharp or throbbing sensations. The effect typically lasts between one and three hours, depending on the drug used and the amount injected.
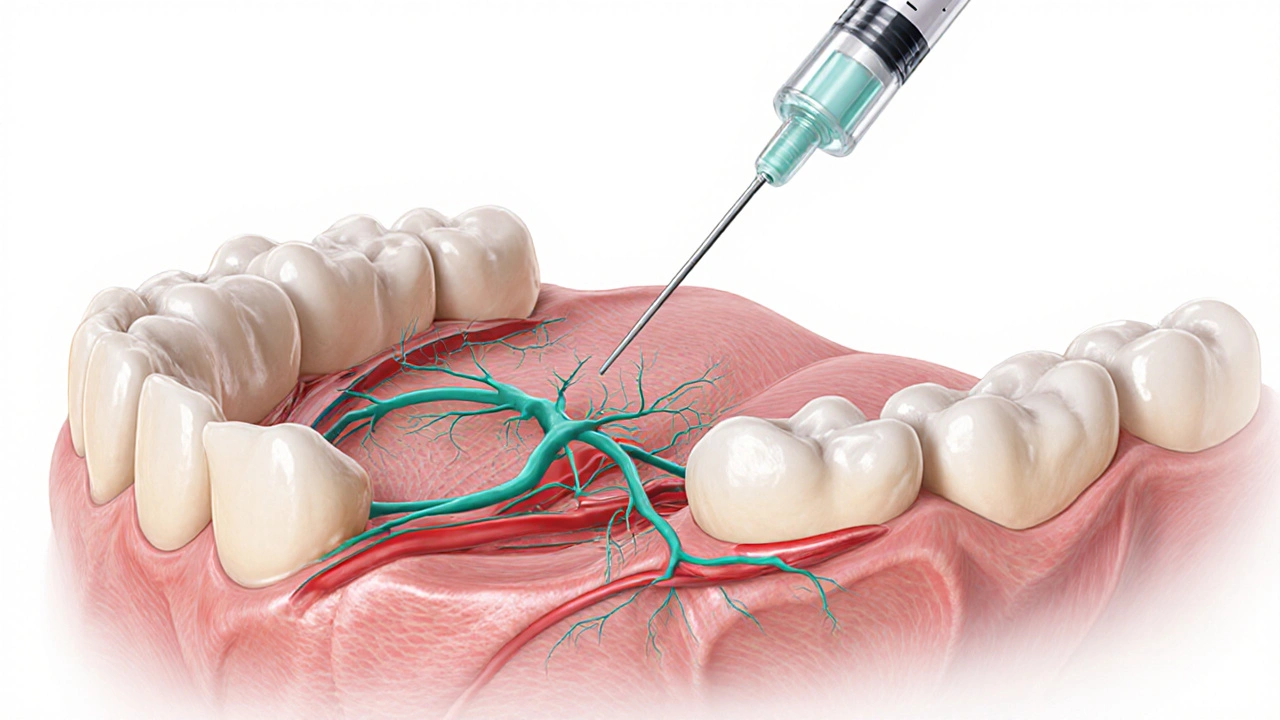
How Does It Work Inside the Mouth?
Dental nerves, especially the inferior alveolar and the mental nerves, carry the bulk of sensation from the lower jaw. When a local anesthetic is injected near these nerves, the active ingredient - usually a molecule like lidocaine - binds to sodium channels on the nerve membrane. This blocks the influx of sodium ions, which is essential for creating the electrical impulse that signals pain.
The addition of a vasoconstrictor (commonly epinephrine) narrows the blood vessels around the injection site. This does two things: it keeps the anesthetic in the area longer, and it reduces bleeding that could dilute the drug. The result is a deeper, longer‑lasting numbness.
Common Dental Anesthetic Agents
Three drugs dominate the dental market today. Each has its own profile for onset (how fast it works), duration (how long the numbness lasts), and maximum safe dose.
| Agent | Typical Concentration | Onset (minutes) | Duration (minutes) | Maximum Dose (mg/kg) |
|---|---|---|---|---|
| Lidocaine | 2% with 1:100,000 epinephrine | 2-4 | 60-120 | 7 |
| Articaine | 4% with 1:100,000 epinephrine | 1-2 | 80-180 | 7 |
| Mepivacaine | 3% (no epinephrine) | 3-5 | 45-90 | 6 |
In head‑to‑head studies, articaine consistently shows the fastest onset and the longest duration, making it a favorite for longer procedures such as root canals. Lidocaine remains the workhorse for most routine work because it has a well‑documented safety record and is available in a wide range of formulations.
What Do the Numbers Say About Pain Reduction?
A systematic review published in the Journal of Dental Research examined 42 randomized controlled trials involving over 5,000 patients. The pooled data revealed an average pain score reduction of 78% when a proper local anesthetic technique was used, compared with placebo or no anesthesia.
One landmark trial from 2022 compared lidocaine and articaine in mandibular molar extractions. Patients rated their intra‑operative pain on a 0‑100 visual analog scale (VAS). The average VAS for lidocaine was 12, while articaine achieved an average of 8 - a statistically significant difference (p<0.01). Importantly, both drugs kept post‑operative pain under 20 on the same scale for the first 24hours.
These findings line up with everyday clinical observations: when the injection hits the nerve bundle correctly, the patient often reports barely feeling the drill, and any residual soreness is usually mild and short‑lived.
Factors That Influence Effectiveness
Even the best drug can fall short if the delivery isn’t spot‑on. Here are the biggest variables that sway the outcome.
- Injection Technique: The inferior alveolar nerve block (IANB) is the gold standard for lower‑jaw work. Studies show a correctly placed IANB reduces pain scores by roughly 30% compared with a simple mucosal infiltrate.
- Anatomical Variations: Some patients have accessory canals or atypical nerve pathways. In these cases, a supplemental intra‑osseous injection may be required.
- Inflammation: Inflamed tissue lowers the pH, making it harder for the anesthetic to cross nerve membranes. Adding a higher concentration of epinephrine or using buffered lidocaine can improve success rates.
- Patient Anxiety: Dental fear triggers the body’s stress response, releasing cortisol that can raise the pain threshold but also amplify the perception of any residual sensation. Pre‑procedure counseling and, if needed, short‑acting anxiolytics improve the overall experience.
- Vasoconstrictor Choice: Epinephrine at 1:100,000 balances a prolonged effect with minimal cardiovascular impact for most adults. For patients with hypertension, a lower concentration (1:200,000) or a vasoconstrictor‑free formulation may be safer, albeit with a shorter duration.

Safety and Side Effects
When administered by a trained dentist, local anesthetics have an excellent safety profile. The most common side effects are mild and transient:
- Temporary tingling or “pins‑and‑needles” feeling that fades as the anesthetic wears off.
- Minor bruising at the injection site.
- Rarely, a prolonged numbness lasting more than 6hours, often due to an inadvertent intravascular injection.
Severe allergic reactions are extremely uncommon, occurring in less than 0.1% of cases. In the unlikely event of an adverse reaction, dentists carry emergency kits with intramuscular epinephrine and antihistamines.
What Patients Can Do to Maximize Comfort
Knowing what to expect and how to prepare can make the difference between a smooth visit and lingering discomfort.
- Share Your Dental History: Mention any previous anesthesia failures, allergies, or cardiovascular conditions before the appointment.
- Stay Relaxed: Deep breathing or listening to calming music reduces stress hormones that can interfere with the anesthetic’s action.
- Follow Post‑Procedure Instructions: Avoid hot foods for the first hour, chew on the opposite side, and keep the mouth clean to prevent infection that could reignite pain.
- Report Numbness Issues: If the area remains numb for more than 6hours or you feel sharp pain despite the injection, call your dentist promptly.
By partnering with your dental team, you help ensure the local anesthesia does exactly what it’s meant to - keep you pain‑free while the dentist does the work.
Frequently Asked Questions
How long does the numbness last after a typical dental injection?
For lidocaine with epinephrine, numbness usually fades between 60 and 120 minutes. Articaine can last up to three hours, especially after longer procedures.
Can local anesthesia cause permanent nerve damage?
Permanent damage is exceedingly rare. Most post‑injection nerve injuries are temporary and resolve within weeks. Proper technique minimizes risk.
Is it safe to take ibuprofen before a dental appointment?
Yes, a dose of ibuprofen taken 30-60 minutes prior can reduce inflammation and improve anesthetic effectiveness, provided you have no contraindications such as stomach ulcers.
Why does my mouth feel “tingly” after the injection?
The tingling is a normal sign that the anesthetic is working on the nerve fibers. It disappears as the drug is metabolized.
Can I request a different anesthetic if I’m allergic to lidocaine?
Absolutely. Alternatives such as mepivacaine or a lidocaine‑free formulation are available. Your dentist will review your medical record to choose the safest option.
Understanding how local anesthesia works, what influences its success, and how to prepare for your appointment puts you in control of the dental experience. Armed with this knowledge, you can walk into the chair with confidence that pain will be kept at bay.


Samantha Dean
Local anesthesia has been a cornerstone of modern dentistry for over a century, and the data presented underscores its remarkable efficacy. By blocking sodium channels in peripheral nerves, agents such as lidocaine and articaine prevent nociceptive transmission with a predictably high success rate. The systematic review you cite, demonstrating an average 78 % reduction in pain scores, aligns with the consensus in the literature. Moreover, the inclusion of vasoconstrictors not only prolongs the anesthetic effect but also minimizes systemic absorption, thereby enhancing safety. It is worth noting that technique, rather than merely the choice of agent, remains the predominant determinant of analgesic outcome. Consequently, clinicians should prioritize precise nerve block placement alongside appropriate drug selection to optimize patient comfort.
James Madrid
Great breakdown! It’s useful to see the numbers laid out so clearly, especially the comparison between lidocaine and articaine. Knowing that articaine can give a faster onset and longer duration helps when planning longer procedures like root canals. Also, the reminder that anxiety levels can shave a few points off the effectiveness is a good nudge to address patient comfort before the injection. Keep the practical tips coming – they make the science feel more applicable.
John Carruth
When I first stepped into a dental surgery, the sterile smell and the hum of the drill made me wonder how much of the process is truly about skill versus chemistry. The local anesthetic, though often taken for granted, is a marvel of pharmacology, engineered to silence pain signals with surgical precision. Its mechanism-binding to voltage‑gated sodium channels-prevents the depolarization that would otherwise trigger an alarm in the brain. The addition of epinephrine acts like a traffic controller, slowing the blood flow so the drug lingers longer where it is needed. In the data you presented, the average pain reduction sits comfortably above three‑quarters, which translates to a dramatic improvement in patient experience. Yet the distribution of that reduction is not uniform; certain procedures, such as deep extractions, still report higher residual discomfort. That residual pain often correlates with factors like tissue inflammation, patient anxiety, and even the exact geometry of the injection site. It is fascinating that a simple change in the angle of the needle can halve pain scores in some studies. Moreover, the choice between lidocaine, articaine, and mepivacaine is not merely a matter of onset and duration; each agent interacts differently with the surrounding vasculature and nerve fibers. For instance, articaine’s higher lipid solubility allows it to penetrate dense bone more effectively, a property that can be decisive in mandibular procedures. Conversely, mepivacaine’s lack of vasoconstrictor makes it a suitable option for patients with cardiovascular concerns, though at the cost of a shorter window of numbness. The clinician’s toolbox therefore includes not only the drugs themselves but also a nuanced understanding of patient-specific variables. This is why continuing education and hands‑on workshops remain essential for dentists who wish to refine their anesthetic technique. In practice, a well‑executed inferior alveolar nerve block can reduce perceived pain by up to 50 %, an outcome that many patients notice and appreciate. It also reduces the need for supplemental intra‑operative analgesics, lowering the overall drug load. Lastly, we should not overlook the psychological aspect: when patients trust that the dentist has mastered both the art and science of anesthesia, their reported pain levels tend to drop even further. In short, local anesthesia is a complex interplay of chemistry, anatomy, and patient psychology, and mastering it yields benefits that extend far beyond the immediate procedure.
isabel zurutuza
Oh great, another chart proving needles work better than they feel.
Justin Valois
Yo, I swear those numbers are legit even if they look like a meme‑filled spreadsheet from the 90s. Articaine's basically the superhero cape for your molar, while lidocaine's the trusty sidekick that never quits. Sure, the charts are messy, but you can't argue with a 78% pain drop – that's like, almost a magic trick, bro. If you ever thought dentistry was just drills and gossip, think again, fam.
Jessica Simpson
In many cultures, the approach to dental pain management intertwines with traditional practices, such as herbal rinses or acupuncture, before modern anesthetics are even considered. Understanding these backgrounds can help clinicians communicate more effectively, especially when patients express hesitation about injection‑based numbing. For example, in certain Indigenous communities, the concept of “numbing” is linked to spiritual balance, so a brief explanation of how the anesthetic works on a physiological level can build trust. Incorporating cultural sensitivity not only improves compliance but also enhances the overall therapeutic alliance, leading to better outcomes.
Ryan Smith
Sure, but you know the big pharma lobby’s quietly pushing these “modern” anesthetics to keep the old herbal tricks out of the market while lining their own pockets. They love a good data point that screams efficiency, even if it means sidelining centuries‑old wisdom that actually works for some folks.
Bill Gallagher
When evaluating the efficacy of local anesthetics, one must consider numerous variables: the pharmacokinetic profile of the agent, the presence or absence of vasoconstrictors, the precise anatomical site of injection, the patient's metabolic rate, and even the ambient temperature of the operatory; each of these factors can significantly modulate the overall analgesic outcome. Moreover, the literature consistently demonstrates that articaine, due to its higher lipid solubility, achieves a more rapid onset-often within one to two minutes-compared to lidocaine, which typically requires two to four minutes; this difference, while seemingly minute, can impact procedural timing and patient comfort substantially. Duration is equally important: articaine can provide numbness for up to three hours in some cases, whereas lidocaine's effects may wane after two, necessitating supplemental dosing in longer procedures. The inclusion of epinephrine, commonly at a concentration of 1:100,000, serves to constrict local blood vessels, thereby reducing systemic absorption and prolonging the anesthetic block; however, this also introduces considerations for patients with cardiovascular sensitivities, who may require alternative formulations. Clinical trials have reported average pain reduction percentages hovering around 78%, yet stratified analyses reveal that anxiety levels, tissue inflammation, and operator technique can cause deviations of ±10% from this mean. Consequently, a comprehensive assessment of the individual patient-encompassing medical history, psychological state, and procedural requirements-is paramount to selecting the optimal anesthetic regimen.
Melodi Young
Thanks for the thorough rundown! It’s helpful to see the specifics broken down, though I think a quick summary chart would make the info even more accessible for busy practitioners.
Tanna Dunlap
It is disconcerting that we continue to tolerate a system where patients are often left to endure unnecessary discomfort because practitioners overlook the ethical imperative to minimize pain. The reliance on chemical numbing without adequate consideration of a patient’s emotional well‑being borders on negligence, and we must hold ourselves to higher standards of compassionate care.
Rajashree Varma
Your concern is valid, and it reminds us that empathy should accompany every injection. By integrating gentle communication, offering clear explanations, and practicing meticulous technique, we can uphold both scientific excellence and moral responsibility, ultimately creating a more humane dental experience.
Anshuman Pandey
Indeed, the act of numbing a tooth is more than a chemical blockade; it reflects the broader principle that we, as caregivers, strive to alleviate suffering wherever it arises. When we view each procedure as an embodiment of mindfulness and intention, the anesthetic becomes a tool for compassion rather than merely a pharmacological convenience.