When your allergies won’t quit-no matter how many antihistamines you take-you might be wondering if there’s a way to actually change how your body reacts. Not just mask the sneezing, but immunotherapy-a treatment that retrains your immune system to stop overreacting to things like pollen, dust mites, or bee stings. This isn’t a quick fix. It’s a long-term strategy. And it works.
How Immunotherapy Changes Your Body’s Response
Allergy shots and sublingual tablets aren’t just another pill or spray. They’re the only treatments proven to alter the immune system’s response to allergens. Instead of fighting symptoms, they slowly expose you to tiny, controlled amounts of what triggers your allergies. Over time, your body learns not to panic. It’s like training a nervous dog: start with a whisper, then a normal voice, until the sound doesn’t scare them anymore.
This method, first used in 1911, is now backed by decades of research. According to the American College of Allergy, Asthma & Immunology (ACAAI), about 85% of patients see major symptom reduction after three years of treatment. That means fewer nasal sprays, less reliance on pills, and in many cases, no more asthma attacks triggered by seasonal pollen.
The key difference between immunotherapy and other treatments? It doesn’t just treat the reaction-it prevents it from happening again. Some people even stop needing medication entirely after finishing the full course.
Allergy Shots: The Gold Standard
Allergy shots, or subcutaneous immunotherapy (SCIT), are still the most effective option. They work for multiple allergens at once. If you’re allergic to grass, ragweed, dust mites, and cat dander, one set of shots can cover them all. That’s huge-because 78% of allergy sufferers react to more than one trigger.
The process has two phases. First, the build-up phase. You get injections once or twice a week, with gradually increasing doses. This lasts 3 to 12 months, depending on the schedule. Then, you move to maintenance: shots every 2 to 4 weeks, for 3 to 5 years total.
There are faster options now. Cluster immunotherapy cuts the build-up time from months to weeks. Instead of weekly visits, you do 8 to 10 appointments over 4 to 9 weeks, with multiple shots per session. Rush immunotherapy-used mostly for life-threatening insect venom allergies-can get you to maintenance in under two months. But even with these shortcuts, you still need the full 3 to 5 years of maintenance shots to get lasting results.
Studies show SCIT reduces symptoms by 82% on average. That’s higher than any tablet. And it’s not just about comfort. Research from the Journal of Allergy and Clinical Immunology says allergy shots can prevent new allergies from developing and even stop allergic rhinitis from turning into asthma.
Sublingual Tablets: Convenience Without Compromise?
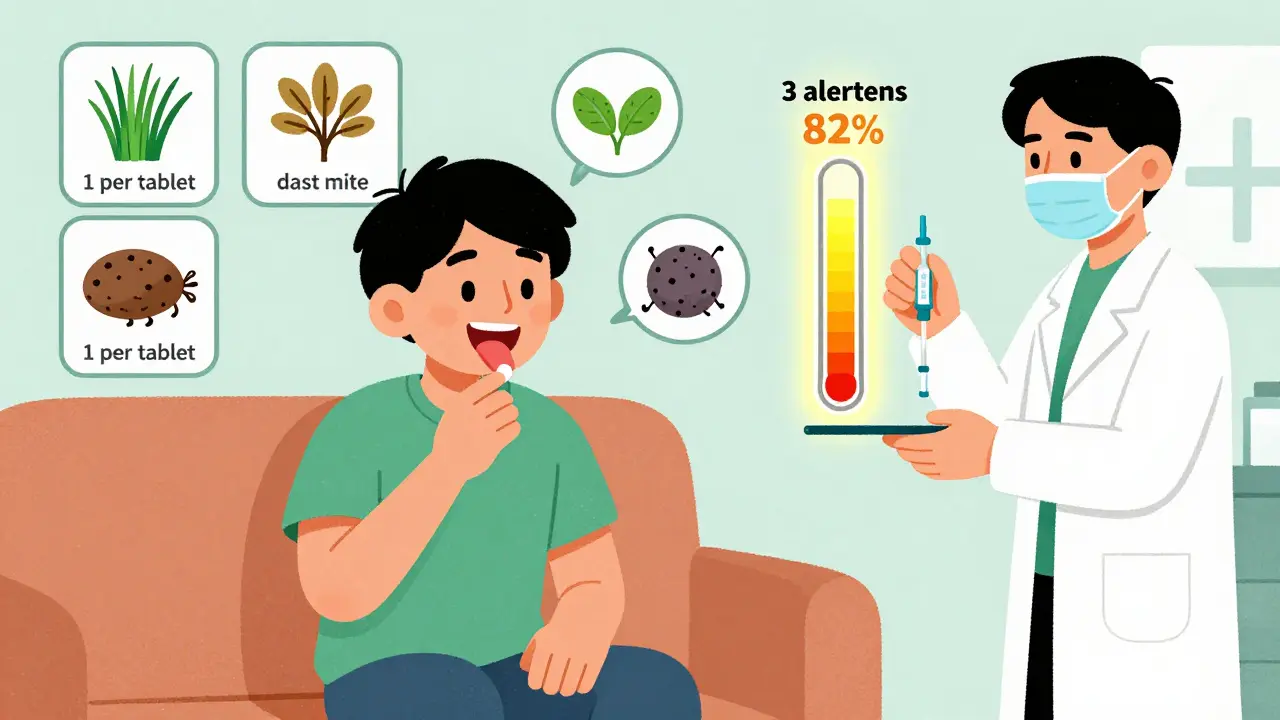
Sublingual immunotherapy (SLIT) tablets are a game-changer for people who hate needles or can’t make weekly doctor visits. You put a small tablet under your tongue once a day. No shots. No clinics. Just a daily routine.
But there’s a catch. Each tablet only works for one allergen. Oralair for grass pollen. Ragwitek for ragweed. Odactra for dust mites. Cat-PAD, approved in April 2024, is the first for cat dander. But if you’re allergic to grass AND dust mites? You’d need two tablets. And they don’t work together. There’s no combo tablet. No multi-allergen option.
That’s why efficacy drops for people with multiple allergies. One 2021 study found SLIT tablets reduced symptoms by 67%-compared to 82% for shots. And 58% of negative reviews on Healthgrades blamed the tablets for not working well enough when multiple triggers were involved.
On the plus side, convenience wins. A 2022 survey found 92% of tablet users preferred them over shots. One user, a traveling salesperson, said: “I couldn’t manage weekly shots, but the tablet fits perfectly in my routine.”
But here’s the catch: you have to take it every single day. If you miss more than 20% of doses, effectiveness plummets to 45%. Setting phone reminders helps-studies show adherence improves by 37% with reminders.
Which One Works Better? The Data Says This
Let’s cut through the noise. Here’s what the numbers show:
| Feature | Allergy Shots (SCIT) | Sublingual Tablets (SLIT) |
|---|---|---|
| Number of allergens covered | 3-4 per vial | 1 per tablet |
| Effectiveness (symptom reduction) | 82% | 67% |
| Treatment duration | 3-5 years | 3-5 years |
| Build-up time | 3-12 months (or 4-9 weeks with cluster) | Starts immediately |
| Administration | Doctor’s office | Home, daily |
| Common side effects | Itching, swelling at injection site; rare systemic reactions | Mild oral itching (28% of users) |
| Best for | Multiple allergies, severe symptoms | Single allergen, convenience-focused |
Experts agree: if you have multiple allergies, shots are the clear winner. Dr. David M. Lang of Cleveland Clinic says SCIT is “the only treatment that modifies the underlying immune response.” Dr. Richard F. Lockey from USF Health puts it bluntly: “The requirement for separate tablets for each allergen makes comprehensive treatment impractical for most patients.”
But if you’re allergic to just one thing-say, grass pollen-and you’re constantly on the move? Tablets win. They’re safer, easier, and good enough.
Real People, Real Experiences
Reddit’s r/Allergies community analyzed over 1,200 posts in 2023. Of those who tried both, 68% said shots worked better. One user, @AllergyWarrior42, wrote: “After 2 years of Grastek tablets with only 30% improvement, I switched to shots and achieved 80% symptom reduction by year 2.”
But another user on Aspire Allergy’s survey said: “I’ve been on the tablet for 18 months. No more sneezing fits at work. I don’t have to take time off to go to the clinic.”
People who quit shots mostly cite scheduling issues. One in three patients drop out because they can’t keep weekly appointments. That’s why clinics now offer cluster protocols-faster, fewer visits. Meanwhile, tablet users who stop usually say it didn’t help enough, especially if they had more than one allergy.

What’s Next? The Future of Allergy Treatment
The field is moving fast. In April 2024, the FDA approved Cat-PAD for cat dander. That’s the first new tablet in years. And it’s not the last.
Multiple-allergen tablets are in Phase 3 trials. If approved by 2025, they could change everything. Imagine one tablet for grass, dust mites, and ragweed. That’s the holy grail.
Even more exciting: peptide-based therapies. These target specific parts of the immune response, not whole allergens. Early results suggest they could cut treatment time from 3-5 years to just 1-2. And doctors are starting to use component-resolved diagnostics-testing for exact proteins you react to-so treatments can be personalized.
But accessibility remains a problem. There are only 5,300 board-certified allergists in the U.S. That means long waits, especially in rural areas. Tablets help bridge that gap. But they’re not a full replacement.
Choosing the Right Path for You
So which one should you pick?
- Choose allergy shots if: You’re allergic to 2+ triggers, your symptoms are severe, you can commit to regular visits, and you want the strongest, longest-lasting results.
- Choose sublingual tablets if: You’re allergic to just one thing, hate needles, travel often, or can’t get to an allergist regularly. But be honest-you have to take it every day.
There’s no shame in either option. Both are scientifically proven. Both can change your life. The difference is in your lifestyle, your triggers, and your willingness to stick with it.
And remember: immunotherapy isn’t about feeling better next week. It’s about feeling better for the next 10 years.
Are allergy shots worth the hassle?
Yes-if you have multiple allergies or severe symptoms. While weekly visits are inconvenient, the long-term results are unmatched. Studies show 85% of patients get major symptom relief after 3 years. Many stop needing daily medication entirely. The upfront effort pays off in fewer sick days, less medication, and better quality of life.
Can sublingual tablets treat multiple allergies?
Not currently. Each FDA-approved tablet targets just one allergen: grass, ragweed, dust mites, or cat dander. If you’re allergic to two or more, you’d need to take separate tablets daily. There’s no combo tablet yet. That’s why shots remain the only option for comprehensive treatment.
How long before I see results from immunotherapy?
You might notice small improvements within 6 to 12 months. But real, lasting change takes time. Most patients see major symptom reduction after 2 to 3 years of treatment. The immune system doesn’t rewire overnight. Stick with it-even if you don’t feel better right away.
Do allergy shots hurt?
The injection feels like a quick pinch, similar to a flu shot. Most people report mild swelling or itching at the injection site, which fades within hours. Serious reactions are rare-about 2% of patients. Clinics monitor you for 30 minutes after each shot to ensure safety.
Is immunotherapy covered by insurance?
Yes, most insurance plans cover both allergy shots and sublingual tablets, especially if prescribed by a board-certified allergist. Out-of-pocket costs vary, but shots are often cheaper over time because they’re administered in-office. Tablets may have higher copays due to brand-name pricing, but no office visits mean savings on time and travel.
Can children do immunotherapy?
Yes. Both allergy shots and sublingual tablets are approved for children as young as 5. Shots are often preferred for younger kids with multiple allergies or asthma risk. Tablets are easier for school-aged children who can manage daily dosing. Always consult a pediatric allergist to determine the best option.
If you’re tired of living with allergies, immunotherapy isn’t a last resort-it’s the most effective solution you haven’t tried yet. Talk to an allergist. Get tested. Find out what you’re really allergic to. Then choose the path that fits your life. Because freedom from allergies isn’t just possible. It’s waiting for you.


Write a comment