Kidney Medication Safety Checker
Check Your Medication Safety
Medication Risk Assessment
When your kidneys aren’t working right, even common medicines can turn dangerous. It’s not about taking too many pills-it’s about your body not being able to clear them. For someone with chronic kidney disease (CKD), a standard dose of ibuprofen, metformin, or even an antibiotic can build up to toxic levels. This isn’t rare. Around 37 million American adults have CKD, and nearly half of them are on 10 or more medications daily for diabetes, high blood pressure, or heart problems. The result? A hidden epidemic of drug toxicity that’s often missed until it’s too late.
Why Kidneys Matter for Medications
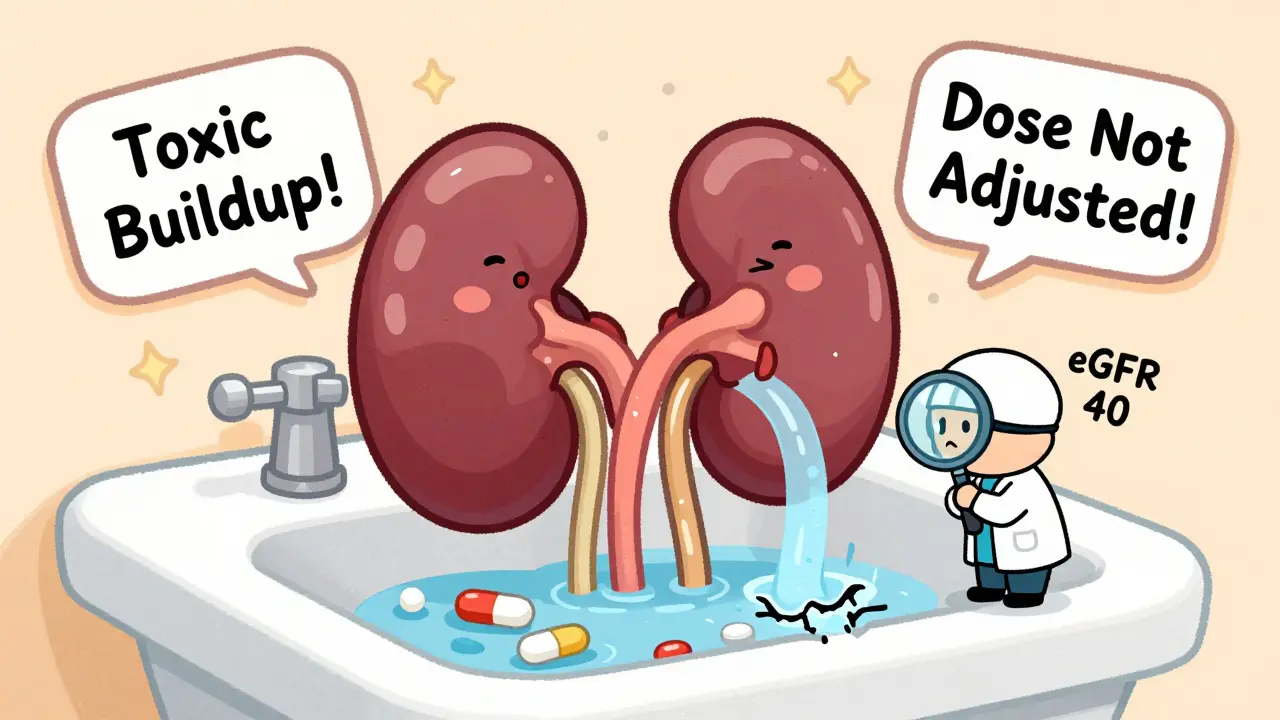
Your kidneys don’t just make urine. They’re your body’s main filter for drugs. About 30% of all medications are cleared directly through the kidneys. Others are broken down by liver enzymes, but their waste products still need to leave the body via urine. When kidney function drops-say, from an eGFR of 90 to 40 mL/min/1.73m²-those drugs stick around. Longer. Stronger. Dangerous.
Think of it like a clogged sink. Water keeps flowing in, but the drain is half blocked. Eventually, it overflows. That’s what happens with medications. Your body keeps giving you the same dose, but your kidneys can’t keep up. The drug builds up. Side effects get worse. And sometimes, the damage becomes irreversible.
Top 5 Medications That Turn Toxic in CKD
Not all drugs are equal when it comes to kidney risk. Some are quietly deadly for people with reduced kidney function. Here are the biggest culprits:
- NSAIDs (ibuprofen, naproxen, diclofenac): These are the most common offenders. They block chemicals your kidneys need to maintain blood flow. In someone with eGFR under 60, NSAIDs can cause acute kidney injury within days. Studies show the risk triples. Many patients don’t even realize they’re taking them-these are over-the-counter painkillers.
- Metformin: Used by 18 million Americans with type 2 diabetes, metformin is generally safe… unless your kidneys can’t clear it. When eGFR drops below 30, the risk of lactic acidosis-a life-threatening buildup of acid in the blood-goes up. But here’s the good news: if you stop it at the right time, the risk drops to near zero. A Cochrane review of 20,000 patients found no lactic acidosis cases when guidelines were followed.
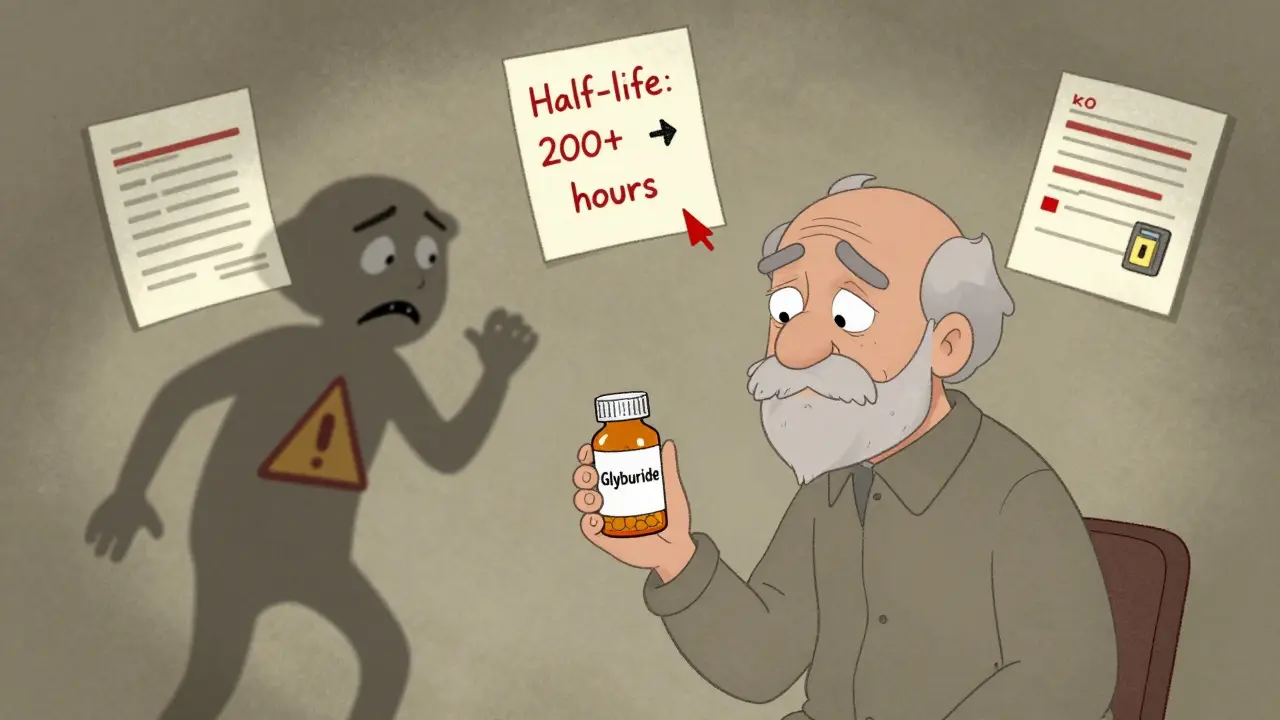
- Sulfonylureas (chlorpropamide, glyburide): These diabetes pills cause low blood sugar. In CKD, they last way longer. Chlorpropamide’s half-life jumps from 34 hours to over 200 hours. Glyburide’s active metabolite sticks around for more than 72 hours. Patients wake up confused, shaky, or unconscious. Glipizide is safer-it doesn’t rely on kidney clearance.
- Trimethoprim (in co-trimoxazole): This antibiotic is often used for UTIs. But when paired with ACE inhibitors or ARBs-common in CKD patients-it can spike potassium levels by 1.2-1.8 mmol/L in just 48 hours. That’s enough to trigger dangerous heart rhythms. One study found a 7-fold increase in hyperkalemia risk.
- Aciclovir: Used for shingles and cold sores, aciclovir can form crystals in the kidney tubules, especially when eGFR is below 50. This leads to crystal nephropathy. About 5-15% of patients develop this, and 20% of those get confused or have seizures from drug buildup.
How Doctors Miss the Signs
Here’s the uncomfortable truth: many doctors don’t check kidney function before prescribing. A JAMA Internal Medicine study found that in 35% of primary care visits, providers used serum creatinine alone-not eGFR-to judge kidney health. That’s like judging a car’s fuel efficiency by looking at the gas tank, not the engine.
Even when eGFR is known, dosing adjustments are often ignored. The American Society of Health-System Pharmacists found a 42% error rate in prescribing renally cleared drugs when eGFR was below 60. Why? Time pressure. Outdated guidelines. Assumptions that “the patient’s fine.”
And it’s not just doctors. Pharmacists miss it too. Patients with CKD often get the same prescriptions as healthy people-until they end up in the ER with acute kidney injury.
Real Stories, Real Consequences
Reddit user ‘KidneyWarrior2022’ posted about taking standard ibuprofen for back pain despite stage 3 CKD. Within 48 hours, their creatinine jumped from 1.8 to 3.2 mg/dL. They were hospitalized for five days. That’s not an outlier. The American Kidney Fund’s forum shows 68% of stage 3-4 CKD patients reported dizziness or confusion from NSAIDs. Over 20% needed emergency care.
Another common story: a diabetic patient on glyburide gets a cold, takes a few extra pills, and collapses from low blood sugar. The doctor says, “You must’ve eaten too little.” But the real issue? The drug was still in their system-long after it should’ve cleared.
One patient on trimethoprim and lisinopril developed potassium levels of 6.8 mmol/L (normal is 3.5-5.0). She had heart palpitations. Her EKG showed dangerous rhythms. She spent three days in the ICU. Her doctor hadn’t checked her potassium in six months.
What You Can Do
You don’t have to wait for a crisis. Here’s how to protect yourself:
- Know your eGFR. Ask for it at every visit. Don’t settle for “your kidneys are fine.” Ask: “What’s my number?” If it’s below 60, ask: “Which of my meds need adjusting?”
- Keep a medication list. Write down every pill, supplement, and OTC drug you take. Bring it to every appointment. Highlight NSAIDs, antibiotics, and diabetes meds.
- Ask about alternatives. If you’re on glyburide, ask about glipizide. If you’re on ibuprofen, ask about acetaminophen. If you’re on trimethoprim, ask if a different antibiotic is safe.
- Use tools. Apps like Meds & CKD (from Healthmap Solutions) scan your meds and flag risks based on your eGFR. Patients using it report 82% better communication with their providers.
- Don’t self-medicate. No NSAIDs without approval. No herbal supplements without checking. Even “natural” remedies like St. John’s Wort or licorice root can harm your kidneys.

The Future Is Better Dosing
There’s hope. In 2023, the FDA approved KidneyIntelX, a machine learning tool that predicts individual toxicity risk with 89% accuracy. Hospitals are starting to use it to flag risky prescriptions before they’re written.
Electronic health records are also getting smarter. Stanford’s Dr. Richard Lafayette predicts that within five years, EHRs will auto-block unsafe prescriptions for CKD patients. That could cut errors by 75%.
And new drugs are being designed with kidney safety in mind. SGLT2 inhibitors like dapagliflozin actually protect the kidneys-but they still need dose adjustments when eGFR drops below 45.
It’s Preventable
Drug-induced kidney injury causes 19-29% of all acute kidney injuries in hospitals. And 65% of those cases are preventable. It’s not about bad luck. It’s about missed checks. Forgotten numbers. Assumptions.
If you have CKD, your kidneys aren’t just weaker-they’re more vulnerable. Every pill you take needs to be reviewed through that lens. You’re not overreacting if you ask, “Is this safe for my kidneys?” You’re being smart.
Because in kidney disease, the right dose isn’t just about effectiveness. It’s about survival.
Can I still take ibuprofen if I have kidney disease?
No-not safely. Even occasional use of ibuprofen, naproxen, or other NSAIDs can cause acute kidney injury in people with CKD, especially if eGFR is below 60. The risk triples. If you need pain relief, acetaminophen (Tylenol) is the safer option, but always check with your doctor first. Never take NSAIDs without knowing your kidney function.
How do I know if my medication dose is too high for my kidneys?
Ask for your eGFR number. If it’s below 60 mL/min/1.73m², your doctor should review all your medications. Look for drugs labeled with “renal adjustment required” or “avoid in CKD.” Common red flags: metformin, sulfonylureas, trimethoprim, aciclovir, vancomycin, and DOACs like apixaban. If your doctor hasn’t mentioned kidney dosing, ask: “Has this been adjusted for my kidney function?”
What’s the difference between eGFR and serum creatinine?
Serum creatinine is a single blood test result-it just tells you how much waste is in your blood. eGFR (estimated glomerular filtration rate) uses that number, plus your age, sex, and race, to estimate how well your kidneys are filtering. Two people can have the same creatinine but very different kidney function. eGFR is the only reliable way to judge kidney health for dosing decisions. Never rely on creatinine alone.
Are over-the-counter supplements safe for kidney disease?
No. Many supplements-like creatine, protein powders, licorice root, and St. John’s Wort-can strain your kidneys or interact with medications. Some contain hidden NSAIDs or heavy metals. There’s no regulation, so safety claims aren’t verified. Always check with your nephrologist or pharmacist before taking anything not prescribed.
Can kidney damage from medication be reversed?
Sometimes. If caught early, stopping the toxic drug and hydrating properly can restore kidney function. But if the damage is severe or lasts too long-like from prolonged NSAID use or crystal nephropathy-it can become permanent. That’s why prevention is everything. Don’t wait for symptoms. Check your eGFR regularly and review your meds before problems start.

Russell Thomas
So let me get this straight - we’re telling people with failing kidneys to avoid ibuprofen, but pharmacists still sell it next to candy bars like it’s aspirin? And doctors don’t even check eGFR? Bro. We’re not saving lives here. We’re running a medical horror show with a PowerPoint presentation.
Joe Kwon
This is such a critical yet under-discussed issue in nephrology. The pharmacokinetics of renally cleared drugs in CKD patients are often overlooked in primary care due to time constraints and fragmented EHR systems. I’ve seen cases where metformin was continued past eGFR <30, and the resulting lactic acidosis required ICU-level intervention. Implementing clinical decision support tools like KidneyIntelX could reduce prescribing errors by up to 70%. We need standardized alerts at the e-prescribing stage - not just guidelines.
Nicole K.
If you're taking NSAIDs with kidney disease, you're basically playing Russian roulette with your organs. It's not just dumb - it's selfish. People don't think about how their choices affect the system. I've seen ERs packed with these cases. Stop being lazy and ask your doctor. That's not hard.
Fabian Riewe
Love this breakdown - seriously, someone should turn this into a printable one-pager for clinics. I’m a nurse and I hand this out to every CKD patient I see. The part about trimethoprim + ACEi causing potassium spikes? That’s a silent killer. I always ask patients: ‘What OTC stuff are you taking?’ and 9/10 say ‘just Advil.’ Just… just stop. Tylenol’s fine. Your kidneys will thank you. 🙏
Teresa Rodriguez leon
I’m a stage 4 CKD patient on dialysis. I used to take glyburide because my doctor said ‘it’s fine.’ Then I passed out at the grocery store. They found my blood sugar at 32. That drug stayed in me for days. I’m on glipizide now. Don’t wait for collapse. Ask. Ask. Ask.
Amy Cannon
It is truly astonishing, and frankly, deeply concerning, that in the United States - a nation with some of the most advanced medical technology on the planet - we still rely on manual, error-prone, paper-based systems to manage medication dosing for chronic kidney disease patients. The fact that serum creatinine is still used as the primary metric, when eGFR has been the gold standard for over a decade, speaks to a systemic failure in medical education and clinical workflow integration. Furthermore, the absence of automated alerts in electronic health records for renally cleared drugs represents a profound lapse in patient safety infrastructure. One must wonder: if this were a car defect, would the NHTSA allow it to remain on the road?
Himanshu Singh
great post! i have CKD and i never knew trimethoprim could raise potassium so fast. i was on it for a UTI last year and felt weird but thought it was just tiredness. now i check my meds with my pharmacist every time. thanks for sharing!!
Jasmine Yule
My mom nearly died from aciclovir toxicity after a shingles outbreak. They didn’t adjust the dose even though her eGFR was 38. She had seizures. The hospital didn’t even have a renal dosing protocol. I’m furious. This isn’t just negligence - it’s malpractice waiting to happen. If you have CKD, don’t trust your doctor. Trust your own research. Print this post. Bring it to every appointment. You are your own best advocate.