Since 2018, a quiet but dangerous problem has shaken the generic drug industry: nitrosamine contamination. These chemicals, found in trace amounts in medicines like blood pressure pills and heartburn drugs, are known to cause cancer-even at levels so small they’re measured in nanograms. What started with a single recall of valsartan has spiraled into one of the largest drug safety crises in modern history. Over 40 specific drug products have been pulled from shelves in the U.S. alone, and more than 500 recalls have been issued by the FDA since then. Generic manufacturers, already operating on razor-thin margins, are now facing a new reality: if your drug contains even a tiny bit of a nitrosamine, it’s not just a quality issue-it’s a public health risk.
What Are Nitrosamines and Why Do They Matter?
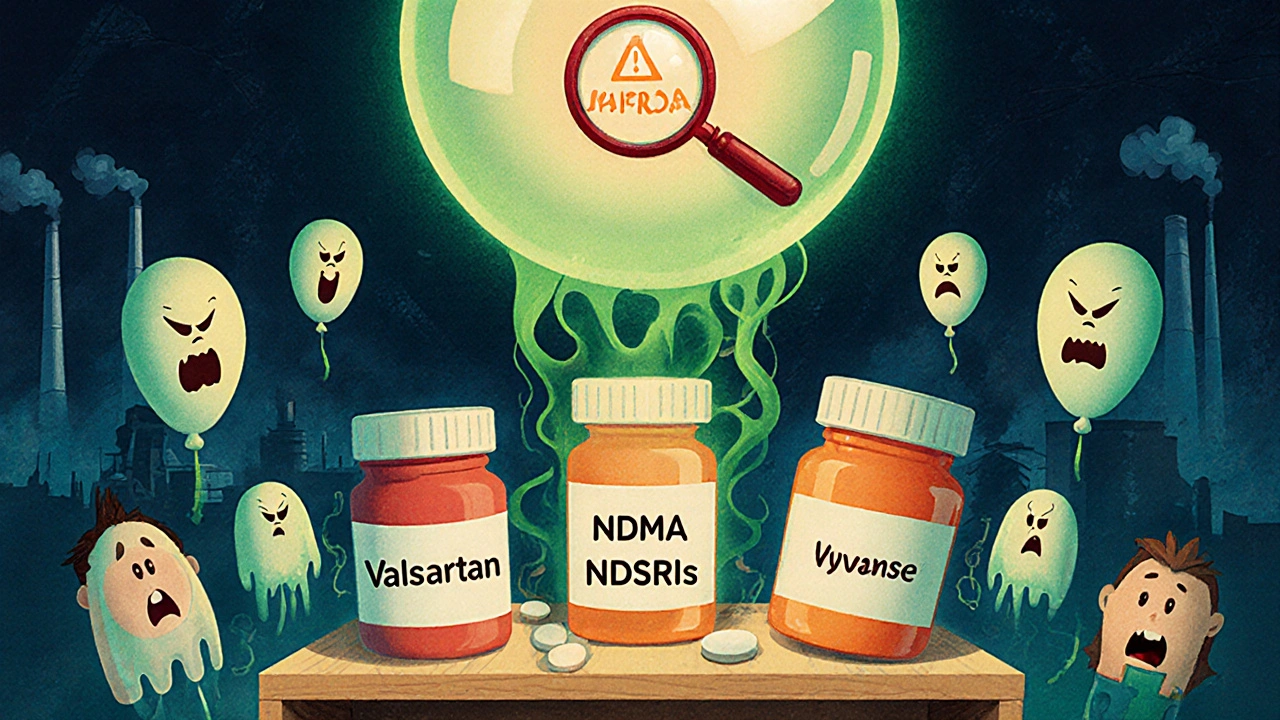
Nitrosamines are a group of chemical compounds that form when certain amines react with nitrites under specific conditions. They’re not added on purpose. They’re accidental byproducts-created during manufacturing, storage, or even from packaging materials. The most common ones found in drugs are NDMA (N-Nitrosodimethylamine), NDEA (N-Nitrosodiethylamine), and newer ones called NDSRIs (nitrosamine drug substance-related impurities), like N-nitroso-varenicline and N-nitroso-duloxetine.
The International Agency for Research on Cancer classifies many of these as probable or possible human carcinogens. That means even long-term exposure to very low doses can increase cancer risk. The FDA’s current acceptable intake limit for NDMA is 96 nanograms per day. To put that in perspective, that’s less than a grain of salt in a swimming pool. But when you’re taking a pill every day for years, those nanograms add up.
Which Drugs Were Affected?
The first wave hit in 2018 with ARBs-angiotensin II receptor blockers used to treat high blood pressure. Valsartan, losartan, and irbesartan were pulled after labs found NDMA and NDEA in their active ingredients. That was just the beginning.
By 2020, ranitidine (Zantac) was pulled globally after tests showed it could form NDMA inside the body over time. Metformin, the most common diabetes drug, followed. Then came antidepressants like duloxetine, smoking cessation aids like varenicline, and even antibiotics and antihypertensives. In 2025, a generic version of Vyvanse was recalled due to NDSRI contamination.
It’s not just the active ingredient. Packaging materials-blister packs, bottle liners, adhesives-have been identified as new sources of contamination. Some blister films contain secondary amines that can react with nitrites from excipients like magnesium stearate, forming NDEA during shelf life. This means a drug can be perfectly clean when made, but turn toxic by the time it reaches the patient.
How the FDA Responded
The FDA moved fast. In 2020, it published detailed testing methods requiring labs to detect nitrosamines at parts per billion levels using LC-MS/MS. In 2023, it released specific acceptable intake limits for each known nitrosamine. For example, NDEA’s limit is 26.5 ng/day, while NDSRIs like N-nitroso-duloxetine are capped at 96 ng/day.
But here’s the catch: if a drug contains more than one nitrosamine, you can’t just add up the individual limits. The FDA says the total exposure must stay below the risk threshold. So if a pill has two nitrosamines, each at 80% of their allowed limit, that’s already 160% of acceptable risk. That’s why many recalls happened even when no single contaminant exceeded its limit.
By 2025, the FDA had issued over 500 recalls tied to nitrosamines. It also began requiring manufacturers to submit risk assessments and control strategies as part of new drug applications. Companies that didn’t have a plan were blocked from getting approvals.
Why Compliance Is So Hard
Fixing nitrosamine contamination isn’t like changing a label. It’s not even just reformulating a drug. It’s rebuilding the entire manufacturing process.
One mid-sized generic maker spent 18 months and $2 million just to fix nitrosamine formation in its metformin line. They had to test every raw material, revalidate every step, and replace suppliers. Another company found that switching magnesium stearate suppliers caused NDEA to form in three different ARB products. They had to overhaul their entire supply chain.
Some manufacturers tried to fix one pathway, only to create a new one. A change in solvent? New nitrosamine. A different drying temperature? Another one. It’s like playing whack-a-mole with chemistry.
Testing alone costs $500,000 to $2 million a year for a mid-sized company. Most small generic makers don’t have the labs, staff, or cash to do it. That’s why the industry is consolidating. Big players like Teva, Sun Pharma, and Fresenius Kabi are surviving. Smaller ones are being pushed out.
Global Differences in Regulation
The FDA isn’t alone, but it’s the strictest. The European Medicines Agency (EMA) has issued 32 recalls. Health Canada, the UK’s MHRA, and Japan’s PMDA have each reported between 5 and 15. But their timelines are more flexible.
The FDA originally demanded full compliance with NDSRI limits by August 1, 2025. That deadline has now been softened. In June 2025, the agency said manufacturers no longer need to meet the full standard by that date. Instead, they must submit progress reports showing they’re actively working on solutions-root cause analysis, reformulation plans, stability data collection.
That change came after industry feedback. FDA officials admitted at the April 2025 Generic Drugs Forum that mitigation strategies vary widely and take years to implement. The agency now recognizes that some companies need more time to gather data, especially for older drugs that weren’t designed with nitrosamine risks in mind.

What’s Next?
Nitrosamines aren’t going away. The FDA has signaled this is a long-term priority. Experts predict more drug classes will be added to the watchlist-possibly antivirals, antifungals, and even over-the-counter pain relievers.
Manufacturers who acted early are now ahead. One company caught a potential nitrosamine risk during development, switched excipients before launch, and avoided a recall entirely. That’s now a case study in FDA training materials.
On the flip side, companies that ignored early warnings are paying the price. Class II recalls mean drugs are pulled immediately. No second chances. And without compliance, new generic applications get rejected.
For patients, the message is clear: don’t panic. The FDA and other regulators are monitoring the situation closely. If your medication was recalled, you were notified. If it wasn’t, it’s likely safe. But the bigger story is about systemic risk in the generic drug supply chain. What’s cheap to make today might be dangerous tomorrow if quality controls aren’t kept up.
How to Stay Safe
If you take a generic drug:
- Check the FDA’s official nitrosamine recalls page regularly. It’s updated weekly.
- Don’t stop your medication without talking to your doctor. The risk from uncontrolled conditions like high blood pressure or diabetes is often higher than the risk from trace nitrosamines.
- If your pharmacy switches your generic brand, ask if it’s the same formulation. A change in manufacturer could mean a new risk profile.
- Report any unusual side effects to your doctor and to the FDA’s MedWatch program.
The bottom line: nitrosamine contamination is a complex, expensive, and ongoing challenge. It’s not a glitch. It’s a structural flaw in how some generic drugs are made-and regulators are finally forcing the industry to fix it.
Are all generic drugs at risk of nitrosamine contamination?
No. Only certain drugs are at risk-mainly those containing amines and exposed to nitrites during manufacturing or storage. Most generic drugs on the market today are safe. The FDA has tested thousands of products and only recalled those with confirmed contamination. If your drug hasn’t been recalled and you’re not on a high-risk list (like ARBs, metformin, or ranitidine), your risk is extremely low.
Can I tell if my medicine has nitrosamines by looking at it?
No. Nitrosamines are invisible. They don’t change the color, smell, or taste of a pill. You can’t detect them without lab testing. The only way to know is through official recalls or statements from your pharmacy or the FDA. Never assume a drug is safe just because it looks the same as before.
Why did it take so long for nitrosamines to be discovered?
Because the testing technology didn’t exist until recently. Detecting nanogram levels of nitrosamines requires advanced instruments like LC-MS/MS, which weren’t routinely used in generic drug quality control until after 2018. Before that, manufacturers tested for known impurities, but nitrosamines were not on the radar. Once sensitive methods were developed, the hidden contamination became visible.
What’s the difference between NDMA and NDSRIs?
NDMA is a well-known nitrosamine that forms from common chemicals like dimethylamine and nitrite. NDSRIs are newer, more complex nitrosamines that form directly from the drug molecule itself. For example, N-nitroso-varenicline comes from the varenicline molecule reacting with nitrites. NDSRIs are harder to predict and control because they’re built into the drug’s structure, not just contaminants from raw materials.
Are brand-name drugs affected too?
Rarely. Brand-name drugs are usually made under tighter controls, with better documentation and more rigorous testing. Most recalls have been for generics, especially those made overseas or by smaller manufacturers. But there have been a few exceptions-like when a brand-name manufacturer used a contaminated excipient. The issue isn’t brand vs. generic; it’s quality control.
What should I do if my drug is recalled?
Don’t stop taking it immediately. Contact your doctor or pharmacist. They’ll help you switch to a safe alternative. For drugs like blood pressure or diabetes medications, stopping suddenly can be dangerous. Your provider will find a replacement that’s been cleared by the FDA. Return the recalled product to the pharmacy or follow FDA instructions for disposal.
Is there a list of safe generic drugs I can trust?
There’s no official "safe list," but you can check the FDA’s recall page and see which products have been cleared after reformulation. Manufacturers that have submitted and received approval for their nitrosamine control plans are more likely to be reliable. Ask your pharmacist if the generic you’re getting has been reformulated since 2023. Many now carry updated labels indicating compliance.

Suzan Wanjiru
Nitrosamines are scary because you can't see them, taste them, or smell them-just take your pill like normal and boom, you're slowly accumulating carcinogens. The FDA's limits are insane-less than a grain of salt in a pool-but when you're on it for decades, it adds up. No wonder people are paranoid.
Jennifer Shannon
You know what’s wild? We’ve been trusting these pills for decades without knowing what was lurking in them. I mean, we assume the FDA is watching, right? But it took advanced tech-like LC-MS/MS-to even *see* these things. Before 2018, we were basically flying blind. And now? Now we’re told to trust the new labels, the new batches, the new suppliers… but how do we know the next batch won’t be the one? It’s not paranoia, it’s just… history repeating. We let cost drive quality, then panic when the cost catches up to us. And the worst part? The people who need these meds the most-elderly, low-income, chronic illness folks-are the ones who get stuck playing Russian roulette with their prescriptions.
I used to think generics were just cheaper versions of the same thing. Now I see them as a gamble with your life. And the companies that cut corners? They’re not evil-they’re just trying to survive in a broken system. But someone’s gotta pay. And it’s not the executives. It’s us.
And don’t even get me started on packaging. Blister packs? Adhesives? Magnesium stearate? I thought those were just filler ingredients. Turns out, they’re chemical time bombs. I read a study where a change in one supplier’s stearate caused NDEA to pop up in three different blood pressure meds. Three! And no one knew until the pills sat on the shelf for six months. That’s not a quality issue-that’s a systemic failure. We need to stop treating drug manufacturing like a commodity market and start treating it like a public health covenant.
I’m not anti-generic. I’m pro-safe. And right now, safe is a luxury. Maybe we need a government-backed generic trust-like a USDA seal for drugs-where only manufacturers who pass third-party, real-time nitrosamine audits get the stamp. Until then, I’m checking the FDA site every week like it’s a lottery ticket. And yes, I’ve switched brands twice. And yes, my pharmacist thinks I’m crazy. But I’d rather be crazy than dead.
Lisa Detanna
It’s not just about the drugs-it’s about who gets left behind when the big players consolidate. Small manufacturers can’t afford $2 million in testing. So they vanish. That means fewer options. Higher prices. And more monopolies. We say we want affordable meds, but we’re making it impossible for anyone but the giants to make them. The FDA’s new flexibility is good, but it’s not enough. We need subsidies. We need public labs. We need to treat drug safety like clean water-something everyone deserves, not something only the rich can afford.
Henrik Stacke
Remarkably, the regulatory evolution here is nothing short of astonishing. One might argue that the FDA’s initial response was overly aggressive, yet the sheer complexity of nitrosamine formation-spanning raw materials, excipients, packaging, and even ambient conditions-demands a nuanced, science-led approach. The shift from rigid deadlines to progress-based reporting reflects a mature understanding of industrial realities. Still, the moral imperative remains: patient safety must never be negotiable, even when compliance is costly.
Jennifer Skolney
Just checked my metformin bottle-new batch, new label says "nitrosamine controlled" 😊 I’m so glad they’re finally fixing this. My dad’s on it and I was terrified. Thanks for the heads-up, OP!
Laurie Sala
I’ve been on valsartan for 12 years… and now I’m supposed to just… trust a new bottle? After what happened? I cry every time I pick it up. I don’t even know if I’m safe. I’m not exaggerating-I have nightmares about this. What if I’ve already damaged myself? What if my kids inherit this? What if the next pill is the one that kills me? Why isn’t anyone talking about the trauma of this? Why is it just… numbers? Nanograms? Recalls? I’m not a statistic. I’m a person who just wants to live without wondering if my medicine is poison.
Matthew Mahar
Wait so if a drug is recalled does that mean the whole batch is bad or just one lot? I got mine from CVS and they just swapped it out but never said why. I think they just swapped the bottle. I mean I dont even know what my pill looks like anymore. I think I need to go back to brand name even if its 10x the cost. I just cant deal with this anymore.
Kezia Katherine Lewis
From a pharmacovigilance standpoint, the emergence of NDSRIs represents a paradigm shift in impurity profiling. Unlike classical process-related impurities, NDSRIs are intrinsic to the drug substance’s molecular architecture, rendering traditional control strategies-such as purification or recrystallization-largely ineffective. The regulatory expectation now requires dynamic, real-time risk assessment frameworks that account for reaction kinetics, excipient interactions, and accelerated stability profiles. This is no longer a QA issue; it’s a molecular engineering challenge.
JD Mette
My mom’s on a generic blood pressure med. She didn’t even know it was recalled until her pharmacist called. She was scared to switch. I had to sit with her for an hour just explaining that the new one was tested and approved. It’s not just about the science-it’s about the fear. And nobody talks about that.
Demi-Louise Brown
Compliance is not optional. The industry must invest in process analytical technology, real-time monitoring, and supply chain transparency. Regulatory agencies must enforce standards uniformly. Patient safety is not a cost center-it is the foundation of pharmaceutical integrity.
John Mackaill
It’s funny how we treat drugs like candy. You get a script, you fill it, you swallow it. No questions. But now we’re learning that even the smallest change-a different supplier, a new drying rack-can turn medicine into a slow poison. I used to think generics were the answer. Now I think they’re the symptom. The real problem is a system that rewards speed over safety. And we’re all paying for it.