Getting the right dose of medicine for a child isn’t just about following a chart. It’s the difference between healing and harm. Every year, thousands of children in hospitals and clinics receive medications based on their weight - not their age. Why? Because a 10-pound baby and a 100-pound teen don’t process drugs the same way. Their bodies are different. Their organs are still growing. And one wrong decimal point can turn a life-saving dose into a dangerous one.
Why Weight Matters More Than Age
For decades, doctors used age to guess how much medicine a child needed. It was quick. Easy. But it was also risky. A 2022 study in Pediatrics showed that using age alone led to medication errors in 29% of cases - especially for kids who were much smaller or larger than average for their age. That’s not a small risk. That’s a preventable danger. Weight-based dosing changed that. Instead of guessing, we measure. We calculate. We use kilograms. The formula is simple: patient’s weight in kg × recommended dose per kg = total daily dose. Then we split it based on how often the medicine is given - once a day? Twice? Three times? Take amoxicillin for an ear infection. The standard dose is 40-50 mg per kg per day, split into two doses. A 10 kg child? That’s 400-500 mg total per day. Divided into two doses? That’s 200-250 mg per dose. Simple. Precise. Safe. But here’s the catch: weight has to be accurate. Not close. Not rounded early. Not in pounds.The Math Behind the Safety
The first step in every pediatric dose calculation? Convert pounds to kilograms. And you do it right - no shortcuts. 1 kg = 2.2 lb. Exactly. No rounding until the very end. If a child weighs 22 pounds, you don’t say “about 10 kg.” You calculate: 22 ÷ 2.2 = 10.00 kg. Keep those two decimal places. Even if the scale only shows whole numbers, the system should store it as 10.00. Why? Because rounding too early causes errors. The Institute for Safe Medication Practices found that 32% of all pediatric dosing mistakes come from incorrect weight conversion. That’s one in three errors - all from skipping a step. Next, multiply the weight (in kg) by the prescribed dose per kg. Then divide by the number of doses per day. That’s your per-dose amount. Example: A 15 kg child needs 15 mg/kg/day of vancomycin, given every 8 hours (three times a day).- 15 kg × 15 mg/kg/day = 225 mg/day
- 225 mg ÷ 3 = 75 mg per dose
When Weight Isn’t Enough: Special Cases
Weight-based dosing works for most kids. But not all. For newborns and infants under six months, kidney and liver function are still developing. A 4 kg preterm baby might need 40-60% less of an aminoglycoside like gentamicin than a full-term infant of the same weight. Weight tells you how big they are. But their organs tell you how fast they clear the drug. For obese children - those with BMI above the 95th percentile - using actual body weight can lead to overdose. That’s because fat tissue doesn’t absorb water-soluble drugs like antibiotics or antivirals. The solution? Use adjusted body weight: Adjusted Body Weight = Ideal Body Weight + 0.4 × (Actual Weight - Ideal Body Weight) This method is now used in 78% of children’s hospitals, according to the Children’s Hospital Association. It’s not just theory. It’s practice. For chemotherapy drugs, body surface area (BSA) is sometimes used instead. The Mosteller formula - √(weight in kg × height in cm ÷ 3600) - gives a more accurate dose for these powerful drugs. But it takes longer. Adds steps. And needs height measurements. That’s why weight-based dosing remains the standard for 87% of pediatric medications.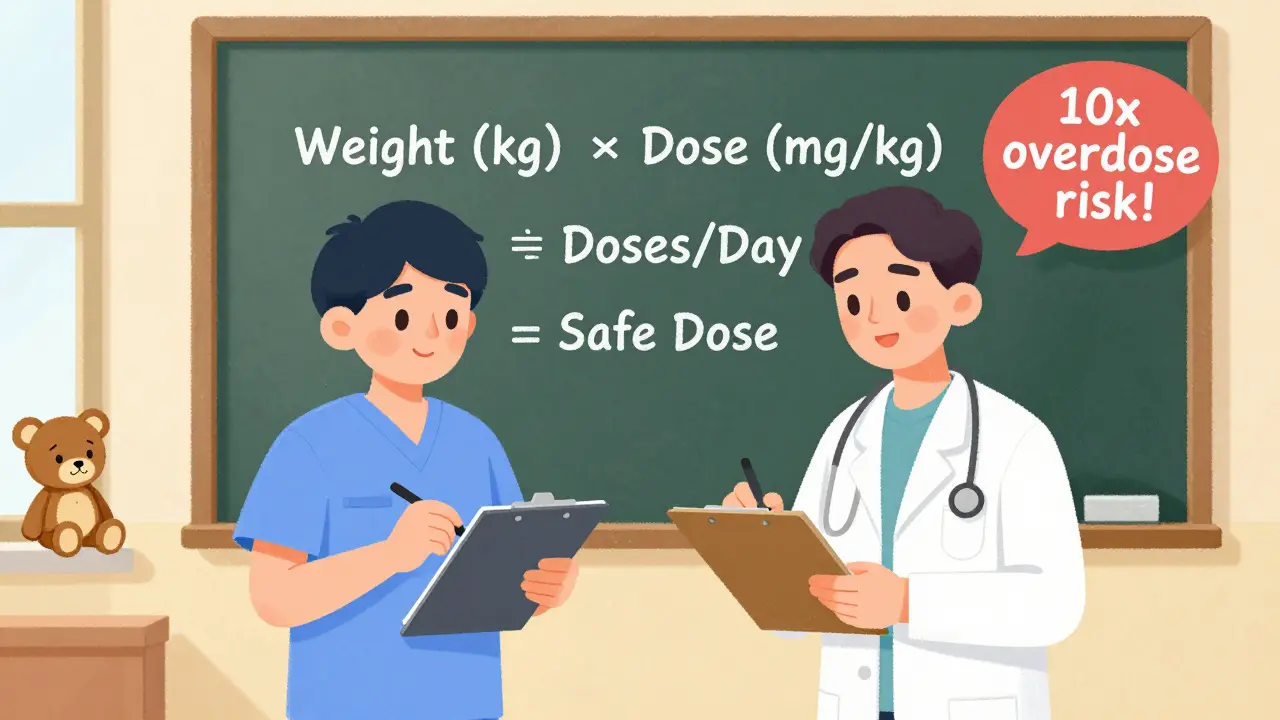
The Double-Check That Saves Lives
Even the best math can fail. A nurse misreads a decimal. A resident types 200 mg instead of 20 mg. A scale is set to pounds instead of kilograms. That’s why the gold standard isn’t just calculation - it’s double-checking. The Joint Commission requires independent double verification for all high-alert medications in children. That means two licensed providers - not one nurse checking their own work - must independently calculate and confirm the dose. A 2023 Medscape survey found that 76% of pediatric nurses say they’ve prevented a near-miss error thanks to this step. One nurse on AllNurses shared: “Last month, we caught a 10-fold overdose on amoxicillin. The resident wrote 200 mg for a 10 kg child. The safe max is 40 mg/kg/day - so 400 mg total. That’s 200 mg per dose. He wrote 200 mg per dose - but forgot to divide by two. We caught it because the dose was double what it should have been.” In emergency rooms, where time is tight, this step can feel like a luxury. But 63% of emergency medicine residents say they’ve seen a near-miss because they skipped the double-check. The cost? Not just time. Sometimes, lives.Technology Is Helping - But Not Replacing
Electronic health records now have built-in dosing calculators. Epic Systems, Cerner, and others auto-calculate doses based on weight. They flag doses that exceed safe limits. Some systems even lock out orders that are too high. In 2023, UCSF Medical Center rolled out a “dose range alert” system. If a dose was more than 10% above or below the expected range for that weight, the system blocked it and required a second approval. Result? A 52% drop in dosing errors. But technology isn’t foolproof. If the weight is entered wrong - say, 22 pounds typed as 22 kilograms - the system will happily calculate a lethal dose. That’s why human verification still matters. Many hospitals now put bright red stickers on scales: “WEIGH IN KG ONLY.” That’s because 38% of all reported dosing errors in 2022 came from using pounds instead of kilograms.What Happens When You Skip the Steps
The numbers don’t lie. In 2022, the Institute for Safe Medication Practices logged 1,247 pediatric dosing errors in U.S. hospitals. The top causes:- Incorrect unit conversion (38%) - pounds vs. kilograms
- Decimal point errors (27%) - 2.0 mg vs. 20 mg
- Failing to adjust for kidney or liver problems (19%)

Training and Standards
Pediatric nurses and pharmacists don’t just learn this once. They’re tested annually. The Pediatric Nursing Certification Board requires a 90% pass rate on a 25-question calculation test. If you don’t hit that, you can’t work with kids until you retrain. Teaching hospitals like Children’s Hospital of Philadelphia use a three-step verification:- Independent weight verification (nurse confirms scale reading)
- Two providers calculate dose separately
- Dose cross-checked against institutional limits
What’s Next?
The future of pediatric dosing isn’t just weight. It’s personalization. The NIH’s Pediatric Trials Network is enrolling 15,000 children to build better dosing rules for common drugs. Genetic testing for drug metabolism - like CYP2D6 and CYP2C19 - is starting to guide opioid and antidepressant dosing in teens. But for now? Weight-based dosing with double-checks remains the foundation. The World Health Organization updated its Essential Medicines List for Children in April 2023 to include weight-band dosing for 127 medications. The FDA now requires pediatric dosing algorithms in all new drug applications by 2025. Dr. Gregory Kearns of the Pediatric Pharmacology Research Unit Network says it best: “While precision dosing through therapeutic drug monitoring will increase, weight-based calculations will remain the essential foundation of pediatric pharmacotherapy for the foreseeable future.”Final Takeaway
Pediatric dosing isn’t complicated. But it’s not simple either. It demands precision, discipline, and a culture of double-checking. One wrong number can hurt a child. One extra step can save them. Use weight. Convert correctly. Calculate carefully. Verify twice. That’s not just protocol. It’s responsibility.Why is weight-based dosing preferred over age-based dosing for children?
Weight-based dosing is preferred because children’s bodies process medications differently based on size, organ maturity, and body composition - not just age. A 2022 study in Pediatrics showed age-based dosing leads to errors in 29% of cases, especially in children who are much smaller or larger than average. Weight-based calculations reduce medication errors by 43% compared to age-based estimates.
How do you convert a child’s weight from pounds to kilograms?
Divide the weight in pounds by 2.2. Always use the exact value without rounding until the final calculation. For example, a child weighing 22 pounds is 22 ÷ 2.2 = 10.00 kg. Rounding too early - like saying 22 pounds is “about 10 kg” - can lead to cumulative errors. Many hospitals now use scales that display weight in kilograms only to prevent this mistake.
What is a double-check protocol in pediatric dosing?
A double-check protocol requires two independent licensed healthcare providers to calculate and verify the dose separately before administration. This is mandatory for high-alert medications in children. The goal is to catch errors like decimal mistakes, wrong units, or misread weights. Studies show this step reduces serious medication errors by 68% in pediatric populations.
Do obese children need special dosing considerations?
Yes. For water-soluble drugs like antibiotics, using actual body weight can lead to overdose because fat tissue doesn’t absorb these medications well. Instead, use adjusted body weight: Ideal Body Weight + 0.4 × (Actual Weight - Ideal Body Weight). This method is used in 78% of children’s hospitals. For fat-soluble drugs, actual body weight may be more appropriate.
What are the most common dosing errors in pediatric care?
The top three errors are: (1) incorrect unit conversion - using pounds instead of kilograms (38% of errors), (2) decimal point mistakes - like 20 mg instead of 2.0 mg (27%), and (3) failing to adjust for kidney or liver impairment (19%). These are preventable with proper training, double-checks, and electronic alerts.
Is body surface area (BSA) better than weight-based dosing?
BSA dosing - calculated using height and weight - is more accurate for chemotherapy drugs because it better reflects metabolic rate. It’s about 18% more precise than weight-based dosing for these medications. But it requires height measurements, takes longer, and is not needed for most drugs. Weight-based dosing remains the standard for 87% of pediatric medications due to its simplicity and reliability.
Are electronic health records enough to prevent dosing errors?
No. While EHR systems now auto-calculate doses and flag unsafe ranges, they rely on accurate input. If a nurse enters a weight of 22 pounds as 22 kilograms, the system will calculate a 10-fold overdose. Technology supports safety, but human verification is still required. Hospitals with both automated alerts and mandatory double-checks have seen error rates drop by over 50%.
What should you do if a child’s weight isn’t measured within 24 hours?
For critical or high-alert medications, weight must be measured within 24 hours of administration. If it’s older, re-weigh the child. Weight can change quickly - especially in sick or dehydrated children. Never assume a weight from days ago is still accurate. This is a Joint Commission requirement for safety.


Angel Tiestos lopez
man i just saw a kid get 10x the dose bc the nurse typed 22 lbs as 22 kg 😭 we gotta do better. why is this still a thing in 2025? 🤦♂️
Pankaj Singh
This is why your ‘modern’ hospitals are still killing kids with incompetence. No one checks the math. No one cares. Just slap on an EHR sticker and call it a day. Pathetic.
Scottie Baker
I’ve seen this happen. A 3-year-old got 200mg of amoxicillin instead of 20mg because someone thought ‘2.0’ meant ‘20’. The mom cried. The nurse quit. The kid survived. But what if they didn’t? This isn’t medicine. It’s Russian roulette with IV bags.
John Tran
You know what’s really tragic? We’ve had the science for decades - weight-based dosing, double-checks, kg-only scales - yet we still treat pediatric care like a high-stakes game of telephone. We’re not just failing kids; we’re failing the very idea of compassion in medicine. It’s not about algorithms or EHRs. It’s about whether we believe a child’s life is worth the extra 30 seconds it takes to verify. And honestly? Most of the time, the answer is no. We’ve normalized risk because it’s easier than accountability. We’ve turned safety into a checkbox. But every decimal point is a heartbeat. And every unchecked box? That’s a future funeral no one wanted to plan.
Angel Molano
If you're not double-checking, you're not a nurse. You're a liability.
Milla Masliy
I work in pediatrics and this is 100% accurate. We weigh every child on arrival, even if they were weighed yesterday. And we always have two people verify high-alert meds. It’s annoying? Yes. But I’d rather be annoyed than bury a kid because we were in a rush.
Avneet Singh
The reliance on weight-based dosing is a heuristic crutch. One must consider allometric scaling, pharmacokinetic ontogeny, and inter-individual variability in CYP450 expression - not just crude kg multiplication. This is reductive pharmacology dressed as protocol.
Nelly Oruko
I’ve been a pediatric nurse for 17 years. I’ve seen 3 near-misses because someone rounded 22 lbs to 10 kg. We now use scales that auto-convert to kg. No decimals. No guesswork. Just science. And yes, we still double-check. Always.
vishnu priyanka
in india we still use age-based dosing in rural clinics… but honestly? most parents bring the kid in with a handwritten note from the local quack saying ‘give 5ml’. so yeah… we just wing it. not proud of it. but real life ain’t a hospital protocol.
Trevor Davis
I used to work ER. We had this one kid come in with a 10x overdose of acetaminophen. Turns out the mom thought ‘10 mg/kg’ meant ‘10 ml’. She used the medicine cup. No scale. No conversion. Just… trust. We saved him. But man. That was a wake-up call.
Anny Kaettano
To every new nurse reading this: the 30 seconds you spend verifying a dose isn’t busywork. It’s the difference between a child going home… and a family never getting closure. You’re not just following protocol. You’re holding a life in your hands. Don’t look away.
Lance Nickie
Weight-based dosing is outdated. Why not use BMI? Or metabolic rate? Or just let AI do it? This whole ‘kg x dose’ thing feels like 1998.