When patients move between hospitals, nursing homes, or even just from the ER to a hospital bed, their medications often get lost in the shuffle. A patient might be taking five pills at home, but the hospital records show only three. One of those missing pills could be a blood thinner. Another could be a heart medication that’s been stopped without anyone noticing. This isn’t just a paperwork error - it’s a recipe for harm. Pharmacist-led substitution programs were built to fix exactly this kind of chaos.
What Exactly Is a Pharmacist-Led Substitution Program?
At its core, a pharmacist-led substitution program is a structured system where pharmacists take the lead in reviewing a patient’s full medication list - at admission, during hospital stay, and at discharge - and making smart, safe changes to improve outcomes. This isn’t just checking if the right pills are being given. It’s about asking: Is this the best drug for this patient right now? Can we switch to a cheaper option? Should we stop something that’s doing more harm than good?
These programs grew out of the 2006 Joint Commission mandate requiring hospitals to reconcile medications during care transitions. But it wasn’t until around 2010-2012 that hospitals realized pharmacists, not just doctors or nurses, were the best people to do this job. Pharmacists know drug interactions, side effects, and therapeutic alternatives better than almost anyone else on the care team. They’re trained to spot when a patient is on a medication that’s no longer needed, when a drug is being duplicated, or when a cheaper, equally effective alternative exists.
How These Programs Actually Work in Practice
It starts with gathering the full medication history. In many hospitals, this is done by trained medication history technicians - not pharmacists - who interview patients, call pharmacies, and check old records. They collect everything: prescription drugs, over-the-counter meds, supplements, even herbal remedies. Then, a pharmacist steps in. They compare this list to what’s in the hospital’s electronic system. On average, they find 3.7 discrepancies per patient. That’s not unusual - it’s the norm.
Once discrepancies are found, the pharmacist decides what to do. Sometimes it’s simple: switch a non-formulary drug to a hospital-approved version. Other times, it’s more complex: stop a proton pump inhibitor that’s been taken for years without clear benefit, or replace an anticholinergic drug that’s increasing fall risk in an elderly patient. In one study, 68.4% of non-formulary medications at admission were successfully substituted with safer, equally effective alternatives.
The process doesn’t end with the hospital stay. At discharge, the pharmacist gives the patient a clear, updated list - written in plain language - and explains what to take, when, and why. They also send this list to the patient’s primary care doctor and community pharmacist. This handoff is critical. Without it, the benefits vanish.
What Results Do These Programs Actually Deliver?
The data speaks clearly. Hospitals with full pharmacist-led substitution programs see:
- A 49% drop in adverse drug events (ADEs)
- A 29.7% reduction in complications like kidney injury or bleeding
- 30-day readmission rates drop by an average of 11% - up to 22% for high-risk patients
- Cost savings of $1,200 to $3,500 per patient from avoided hospitalizations
One standout example is the OPTIMIST trial, which compared standard care to a full pharmacist intervention. The group with pharmacist-led substitutions had a 38% lower risk of being readmitted within 30 days. That means for every 12 patients treated this way, one hospital readmission was prevented.
Deprescribing - stopping unnecessary drugs - is where these programs really shine. In a study of elderly patients, pharmacists recommended stopping anticholinergic drugs in 52% of cases. When followed through, this led to a 41% reduction in falls. In another, stopping long-term proton pump inhibitors reduced C. difficile infections by 29%.
Why Pharmacists? Why Not Doctors or Nurses?
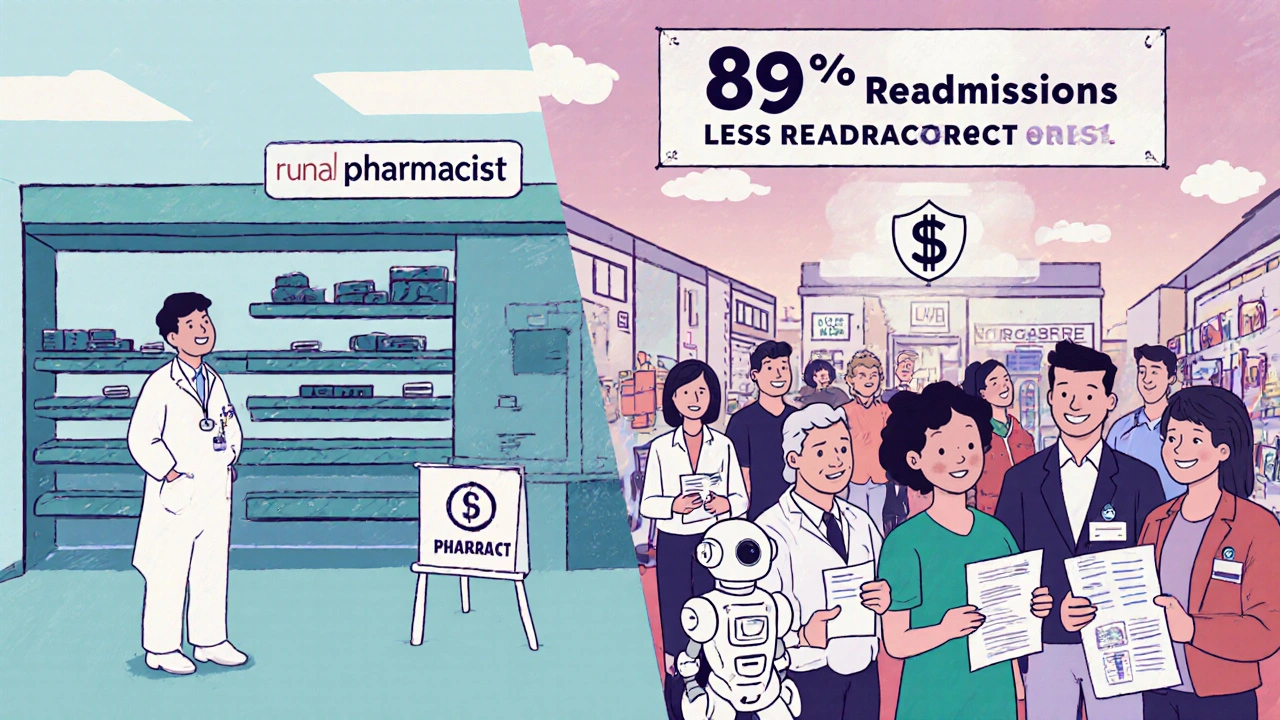
Doctors are busy. Nurses are stretched thin. Pharmacists are the only ones whose entire training focuses on medications - from chemistry to clinical use to cost-effectiveness. A systematic review of 123 studies found that 89% of pharmacist-led programs reduced readmissions, compared to just 37% of non-pharmacy-led efforts.
It’s not just about knowledge - it’s about time and focus. Pharmacists can spend 60-70 minutes per patient reviewing medications. Most physicians don’t have that kind of time during a 15-minute admission round. Nurses may catch a missing pill, but they rarely know if a drug should be stopped entirely or replaced with something safer.
And it’s not just hospitals. Skilled nursing facilities saw a jump from 18% to 42% adoption of pharmacist-led deprescribing programs between 2020 and 2023. That’s because pharmacists can identify drugs that are no longer needed - like statins for terminally ill patients, or blood thinners after a stroke has resolved.
The Big Barriers - And How Top Programs Beat Them
It’s not all smooth sailing. The biggest roadblock? Physician resistance. In 43% of academic hospitals, doctors ignore pharmacist recommendations - especially when it comes to stopping medications. Why? Sometimes it’s habit. Sometimes it’s fear of liability. Sometimes it’s just not on their radar.
Successful programs solve this with technology and protocol. Instead of asking, “Can we stop this?” they use EHR alerts that say: “Patient on PPI for 5 years - no GI diagnosis. Consider deprescribing.” These alerts come with evidence-based guidelines attached. When the recommendation is embedded in the workflow, acceptance jumps.
Time is another problem. A full medication review takes over an hour per patient. To fix this, top programs use a team model: technicians gather data, pharmacists make decisions. One hospital uses two full-time technicians Monday-Friday and 12 interns on weekends. That way, pharmacists aren’t stuck doing data entry - they’re doing what they’re trained for: clinical judgment.
Reimbursement is still a mess. Only 32 states fully reimburse pharmacist-led substitution services through Medicaid. Medicare Part D covers some services, but the paperwork is so heavy that many pharmacists can’t afford to bill for it. Still, the market is growing fast - hitting $1.87 billion in 2022 and projected to hit $3.24 billion by 2027.
The Future: AI, Policy, and Broader Access
The next wave is digital. AI tools are now being tested to auto-populate medication histories from pharmacy records, reducing data collection time by 35%. These tools are piloted at 14 major hospitals and show real promise. In 2024, CMS proposed new rules that would make it easier for pharmacists to document substitutions and get paid for them - potentially boosting reimbursement by 18-22%.
Legislation is catching up too. The 2022 Consolidated Appropriations Act now requires medication reconciliation for all Medicare Advantage patients. That’s a $420 million market opportunity - and it’s forcing hospitals to take these programs seriously.
But access remains unequal. In urban academic centers, 89% have full programs. In rural critical access hospitals? Only 22%. The reason? Pharmacist shortages. You can’t run a substitution program without pharmacists. And in many small towns, there just aren’t enough.
The solution? Expanding scope of practice. Twenty-seven state pharmacy associations are lobbying to let pharmacists initiate substitutions without physician approval - something already allowed in some states for vaccines and naloxone. If that expands, these programs could reach far beyond hospital walls.
What’s Next for Patients and Providers?
Pharmacist-led substitution programs aren’t a nice-to-have. They’re a safety net. They prevent harm. They save money. They reduce readmissions. And they work - especially for the most vulnerable: seniors on five or more drugs, people with poor health literacy, those switching care settings.
For hospitals, the choice is clear: invest in pharmacists, or pay more in penalties. CMS’s Hospital Readmissions Reduction Program fines hospitals for high readmission rates. Those with pharmacist-led programs pay 11.3% less in penalties.
For patients, it means fewer side effects, fewer trips back to the ER, and a medication list they actually understand. For pharmacists, it’s recognition - finally - as essential members of the care team, not just pill counters.
The evidence is solid. The models are proven. The only thing left is scaling them - and making sure every patient, no matter where they live or what hospital they enter, gets the same level of protection.
What is the main goal of pharmacist-led substitution programs?
The main goal is to improve patient safety by identifying and correcting medication errors during care transitions - like hospital admission or discharge. Pharmacists review all medications a patient is taking, spot unnecessary or harmful drugs, switch to safer or cheaper alternatives, and stop medications that are no longer needed. This reduces adverse drug events, prevents hospital readmissions, and cuts healthcare costs.
How do pharmacist-led programs differ from doctor-led medication reviews?
Doctors often focus on diagnosing and treating conditions, while pharmacists specialize in medications. Pharmacists spend more time reviewing every drug - including over-the-counter and supplements - and know which ones interact, which are outdated, and which can be safely stopped. Studies show pharmacist-led programs reduce readmissions 89% of the time, compared to just 37% for non-pharmacy-led efforts. Pharmacists also work with technicians to gather full medication histories, freeing them to focus on clinical decisions.
Do these programs actually save money?
Yes. On average, each patient saves between $1,200 and $3,500 by avoiding preventable hospitalizations or emergency visits. Hospitals also face lower penalties under CMS’s Hospital Readmissions Reduction Program - those with pharmacist-led programs pay 11.3% less. The U.S. market for these services hit $1.87 billion in 2022 and is expected to grow to $3.24 billion by 2027, showing strong financial value.
What’s deprescribing, and why is it important?
Deprescribing means safely stopping medications that are no longer needed or are doing more harm than good. For elderly patients, this often means stopping long-term proton pump inhibitors, anticholinergics, or blood thinners after a stroke has resolved. In one study, deprescribing reduced falls by 41% and C. difficile infections by 29%. Pharmacists are trained to identify these cases and recommend discontinuation - but physician buy-in remains a challenge.
Why aren’t these programs available everywhere?
The biggest barriers are staffing and reimbursement. Running these programs requires trained pharmacists and technicians - in short supply, especially in rural areas. Only 22% of critical access hospitals have full programs, compared to 89% in urban academic centers. Also, Medicare and Medicaid reimbursement is inconsistent - only 32 states fully pay for these services. Without proper payment, many hospitals can’t justify the cost.
Are pharmacy technicians reliable in these programs?
Yes - but only with proper training. Studies show that after two hours of classroom instruction and five eight-hour supervised shifts, pharmacy technicians achieve 92.3% accuracy in collecting medication histories. Their role is to gather data - not make clinical decisions. Pharmacists then review and act on that data. When roles are clearly defined, the system works well.


archana das
Wow, this is the kind of system that could change lives in places like India too. So many people here take five medicines because three doctors told them to - no one ever asks if they still need them. Pharmacists here are usually just dispensing, not thinking. But imagine if they could stop the statins for grandma who’s 90 and barely eats anymore. That’s not just savings - that’s dignity.
Tom Shepherd
so like… if a pharmacist can stop a ppi that’s been going for 5 years, why do docs still write it? i’ve seen the same script for 8 years straight. someone’s asleep at the wheel.
Jauregui Goudy
This is the single most underappreciated revolution in healthcare. We treat pharmacists like glorified cashiers, but they’re the only ones who actually know what’s in those pills - and more importantly, what shouldn’t be in them. The fact that we still need to argue that pharmacists should be allowed to do their job is absurd. These programs don’t just save money - they save people from being turned into pill zombies.
Frances Melendez
Of course it works. It’s obvious. But you know who doesn’t want this? The doctors who get paid for prescribing. And the pharmaceutical reps who still show up with free pens and lunch vouchers. This isn’t about science - it’s about power. And until we cut the ties between drug companies and prescribers, this will always be a fight.
Rhiana Grob
I’ve worked in three different hospitals, and I’ve seen this firsthand. The pharmacist who caught that I missed a beta blocker in a post-MI patient? She saved his life. Not me. Not the attending. Her. And yet, when we tried to expand the program, administration said ‘we don’t have the budget.’ We have the budget for another CT scanner. Not for the person who prevents the ER visits that the scanner is used for. The math doesn’t lie - but someone’s still choosing to ignore it.
Rebecca Price
Let’s be real - this isn’t about ‘substitution.’ It’s about autonomy. Pharmacists are the only clinicians trained to question the entire regimen, not just add to it. And yet, we still treat them like order-takers. Imagine if we let nurses prescribe antibiotics or physical therapists order MRIs. We’d call it ‘overstepping.’ But when a pharmacist says ‘stop this,’ it’s ‘just a suggestion.’ It’s not about training - it’s about hierarchy. And hierarchy kills patients.
Emma Dovener
My mom was on seven meds before her hospital stay. After the pharmacist reviewed everything, three were stopped - including that daily aspirin she’d been taking since 2010. She’s been fine since. No bleeding, no confusion, no extra trips to the pharmacy. It’s not magic. It’s just someone paying attention.
shawn monroe
AI-driven med reconciliation is the future. We’re already piloting NLP models that parse pharmacy logs, EHR notes, and even patient voice recordings to auto-generate med histories. Accuracy’s at 91% with human oversight. The bottleneck isn’t tech - it’s legacy workflows and physician ego. We can automate the grunt work. What we can’t automate is changing a culture that still thinks ‘MD’ means ‘Medication Decider.’
Miriam Lohrum
It’s funny - we spend billions on fancy AI diagnostics, but the most powerful tool we have is a pharmacist with a clipboard and 45 minutes. We’ve outsourced critical thinking to algorithms, but the real intelligence is still human - and it’s sitting in the pharmacy, quietly fixing what everyone else missed.
Jonah Thunderbolt
Let’s be honest - if you’re not using AI to auto-flag deprescribing candidates, you’re basically practicing medieval medicine. And if your hospital still has pharmacists doing data entry? You’re not just inefficient - you’re unethical. This isn’t 2012. We have the tools. We have the data. We have the evidence. What we don’t have? Leadership with a spine.
Sue Haskett
And yet… here’s the thing: no one ever talks about the emotional labor. The pharmacist who spends an hour explaining to an 82-year-old widow why she doesn’t need her blood thinner anymore - because the stroke was 5 years ago, and the risk of bleeding now outweighs the benefit - that’s not a task. That’s a conversation. That’s grief. That’s dignity. And no one tracks that. No one pays for that. But it’s the reason these programs work. Not the algorithms. Not the savings. The humanity.