Quick Takeaways
- Mixing phenazopyridine alcohol interaction can increase dizziness, low blood pressure, and stomach irritation.
- The drug is metabolized by the liver, and alcohol competes for the same enzymes, slowing clearance.
- Even small amounts of alcohol may amplify side effects, especially in people with liver issues.
- If you’ve already combined them, hydrate, monitor symptoms, and contact a healthcare professional.
- Consider non‑alcoholic pain‑relief options for urinary tract infection (UTI) discomfort.
What is Phenazopyridine?
When treating a painful urinary tract infection, many doctors prescribe Phenazopyridine is a synthetic azo dye used as an oral analgesic for urinary tract pain. It works by soothing the lining of the urinary tract, giving relief from burning, urgency, and flank pain. The medication typically comes in 100 mg or 200 mg tablets and is meant for short‑term use-usually no longer than two days-because it does not treat the infection itself, only the discomfort.
How Alcohol Affects Your Body
Alcohol is a volatile compound that the liver breaks down primarily via the enzyme family cytochrome P450 (especially CYP2E1). While moderate drinking can be tolerated by many, the process creates acetaldehyde, a toxic metabolite that can damage liver cells and alter blood‑brain barrier function. This is why drinking, even in modest amounts, can cause dizziness, impaired coordination, and changes in blood pressure.
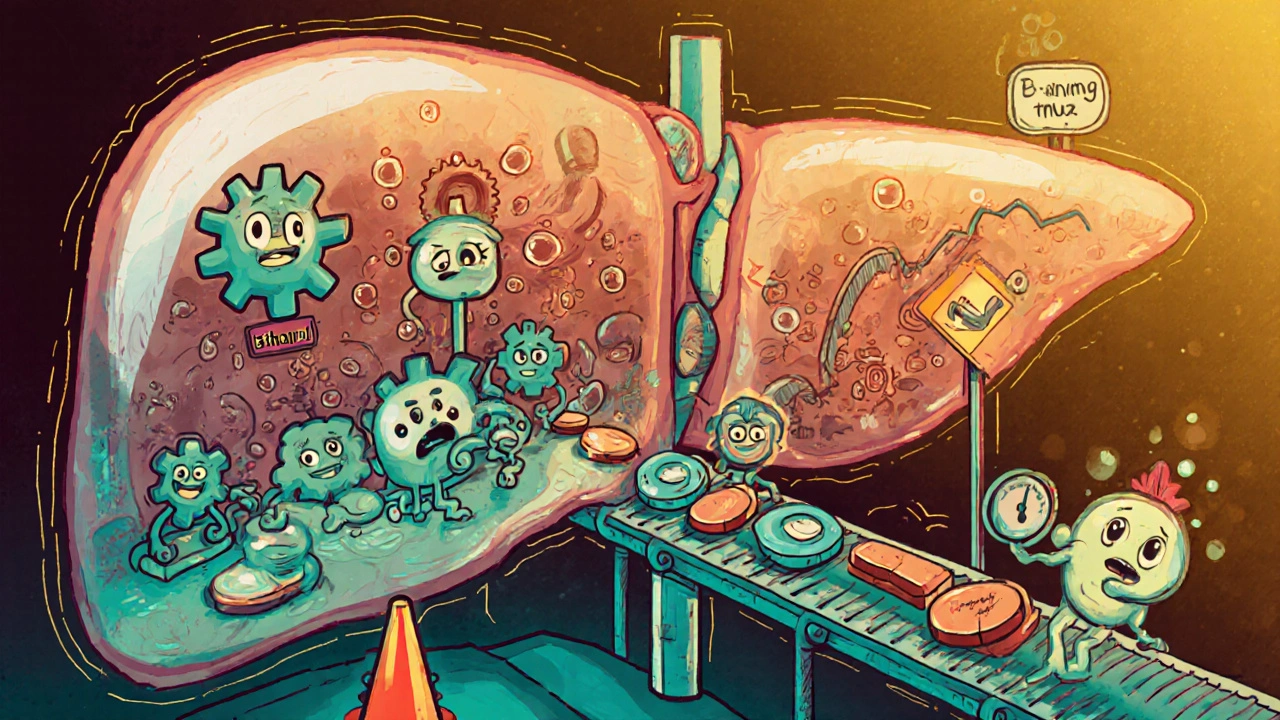
Why Mixing Matters: Metabolism & Liver Interaction
Both phenazopyridine and alcohol rely on the liver for clearance. The liver’s Cytochrome P450 enzymes are a shared highway for many drugs and substances. When you consume alcohol, the enzyme pool is busy processing ethanol, which slows the metabolism of phenazopyridine. The result? Higher blood levels of the drug for a longer period, which can magnify its side effects.
In people with pre‑existing liver conditions-such as hepatitis, fatty liver disease, or chronic alcohol use-the risk spikes further. The liver may not clear either substance efficiently, leading to a buildup of both acetaldehyde and phenazopyridine metabolites, potentially causing nausea, vomiting, and a dangerous drop in blood pressure (hypotension).
Potential Side Effects and Risks
When phenazopyridine is taken alone, common side effects include:
- Mild nausea
- Headache
- Orange‑red urine (harmless but can stain clothing)
Adding alcohol can intensify these and introduce new issues:
- Dizziness - the combined depressant effect on the central nervous system can make you feel light‑headed even after a single drink.
- Low Blood Pressure - both substances can cause vasodilation; together they may lead to fainting.
- Stomach Irritation - phenazopyridine can be harsh on gastric lining, and alcohol increases stomach acid production.
- Increased Risk of Overdose - because clearance slows, taking the usual dose may unintentionally become a higher effective dose.
- Exacerbated Flank Pain - paradoxically, the drug’s intended pain relief can be masked, making it harder to gauge symptom improvement.
These risks are especially relevant for older adults, pregnant individuals, and anyone taking other medications that also use the CYP pathway.
Safe Guidelines & What to Do If You’ve Mixed
If you plan to take phenazopyridine, the safest bet is to avoid alcoholic beverages altogether during the course of treatment. Here’s a quick rule‑of‑thumb:
- Finish the prescribed phenazopyridine course (usually 2 days).
- Refrain from alcohol for at least 24 hours after the last dose.
- If you accidentally have a drink, stay hydrated-water helps the kidneys flush both substances faster.
- Monitor for red‑flag symptoms: severe dizziness, fainting, persistent vomiting, or a rapid heart rate.
- Contact a healthcare professional right away if any red‑flag symptom appears.
For those who have already mixed the two, the following steps can reduce harm:
- Hydration: Aim for 2‑3 liters of water over the next 12 hours.
- Food: Eat a balanced meal to slow further absorption.
- Rest: Sit or lie down if you feel dizzy; avoid driving.
- Medication Review: Inform your pharmacist or doctor about the mix; they may adjust future dosing or suggest an alternative analgesic.

Managing UTI Pain Without Alcohol
If you need to avoid alcohol, there are several proven strategies to keep UTI discomfort under control:
- Increase fluid intake-cranberry juice (unsweetened) or plenty of water helps flush bacteria.
- Heat therapy: a warm sit‑z‑bath can soothe bladder spasms.
- Over‑the‑counter Analgesics such as ibuprofen (if not contraindicated) can reduce inflammation and pain.
- Probiotic foods (yogurt, kefir) may promote a healthy urinary microbiome.
- Follow the full antibiotic regimen prescribed for the infection; pain relief will be short‑lived once the infection clears.
Risk Comparison Table
| Alcohol Amount | Expected Effect | Risk Level | Recommendation |
|---|---|---|---|
| None | Standard drug clearance | Low | Proceed as prescribed. |
| 1‑2 standard drinks (within 2 hrs) | Minor slowdown in metabolism | Moderate | Consider delaying dose or choosing an alternative. |
| 3+ drinks or binge drinking | Significant enzyme competition, higher drug plasma levels | High | Avoid mixing; seek medical advice if already combined. |
Frequently Asked Questions
Can I have a single glass of wine while taking phenazopyridine?
A single glass (about 5 oz) may still interact, especially if you have a sensitive liver. The safest approach is to skip alcohol until the medication course ends.
Why does my urine turn orange after taking phenazopyridine?
The drug’s dye is excreted unchanged, giving urine a reddish‑orange hue. It’s harmless but can alarm people who aren’t expecting it.
What should I do if I feel dizzy after mixing the two?
Sit or lie down, drink water, and avoid driving. If dizziness persists beyond 30 minutes or you feel faint, call your doctor or go to urgent care.
Are there any long‑term risks from a one‑time mix?
A single accidental mix is unlikely to cause lasting damage in healthy adults, but repeated interactions can strain the liver and raise the chance of chronic issues.
Can I take phenazopyridine with non‑alcoholic beer?
Non‑alcoholic beer usually contains less than 0.5% alcohol, which is generally safe. Still, monitor how you feel and keep hydration high.


Dahmir Dennis
So you think popping a couple of drinks while taking a cheap over‑the‑counter urinary analgesic is a brilliant idea? Well, let me enlighten you about the magnificent symphony of metabolic chaos you’re about to conduct. Phenazopyridine, that orange‑tinged miracle, already hangs around your bloodstream long enough to annoy your kidneys. When you invite ethanol to the party, the cytochrome P450 enzymes have the courtesy of playing traffic cop for a whole afternoon. The result is nothing short of a pharmacokinetic traffic jam, and you, dear reader, become the unwitting victim of elevated drug concentrations. Elevated levels mean amplified dizziness, the delightful sensation of being a newborn fawn on ice. Add to that the seductive drop in blood pressure, which makes you feel as if gravity has been personally offended by your existence. Your stomach, already irritated by the dye, receives a complimentary injection of acid thanks to alcohol’s mischievous stimulation of gastric secretions. And let’s not forget the charming orange urine, now glowing like a traffic signal warning others to stay away. You might think a single glass of wine is harmless, but the liver, that overworked detox factory, doesn't care about your social etiquette. It will prioritize ethanol, leaving phenazopyridine to loiter, increasing the odds of an accidental overdose. This is the perfect recipe for a teeter‑to‑tumble episode where you might faint in the bathroom, clutching a porcelain throne. If you happen to be older or have a tender liver, the odds become a ruthless roulette wheel spinning toward catastrophe. Pregnant individuals should be especially vigilant, because the fetus does not appreciate a cocktail of toxins. Bottom line: the safest choice is to abstain, hydrate like a camel, and let the drug do its fleeting job without your drunken interference. Or, if you insist on reckless bravado, at least have an ambulance on speed‑dial, because you'll need one.
Jacqueline Galvan
When using phenazopyridine, it is prudent to avoid alcohol to minimize adverse interactions. The liver’s cytochrome P450 system metabolizes both agents, leading to potential accumulation of the analgesic. Maintaining adequate hydration supports renal excretion and can alleviate mild dizziness. Should any symptoms such as persistent hypotension or severe nausea arise, contacting a healthcare professional promptly is advisable. Following the recommended 24‑hour alcohol‑free interval after the final dose ensures optimal drug clearance.
Amanda Vallery
Yo, dont mix that med with booze. It'll mess up ur liver big time.
Marilyn Pientka
The pharmacodynamic interplay between phenazopyridine and ethanol constitutes a quintessential example of competitive inhibition within the hepatic CYP450 isoenzyme milieu. By allocating enzymatic capacity to ethanol oxidation, substrate turnover of the azo‑dye analgesic is attenuated, precipitating supratherapeutic plasma concentrations. Clinically, this manifests as orthostatic hypotension, vestibular disturbances, and potentiated gastric mucosal irritation. It is incumbent upon the prescriber and patient to adhere to strict abstinence protocols during the therapeutic window.
Jordan Levine
I can't believe people actually think it's okay to drink while on this damn pill 😂😂 It's like inviting a tornado into a paper factory – total disaster! If you want to stay standing, put the wine down and the water up! 🍻
Michelle Capes
I totally get how overwhelming this can feel 😊 staying hydrated and taking it easy is the best move right now. If the dizziness sticks around, don't hesitate to call your doctor – they're there to help.
Dason Avery
Life is a series of choices, each with its own ripple effect 🌊 Choosing to mix phenazopyridine with alcohol is like tossing a stone into still water, the waves may surprise you. Embrace the wisdom of patience and let the medication run its course unaccompanied. In the end, harmony returns when we respect our body's boundaries 🌟
Teya Arisa
It is commendable that you are seeking clarification on this matter. Adhering to a strict no‑alcohol policy during phenazopyridine therapy minimizes risk and promotes recovery. Should any concerning symptoms develop, please seek medical attention without delay 😊
Kester Strahan
Yo, the enzyme competition is legit – the CYP2E1 gets clogged and phenazopyridine hangs longer. This can lead to, like, higher plasma levels and nastier side effects. So ditch the brew while you're on the med, ya hear? It’s simple math: less alcohol equals less risk.
Doreen Collins
Your concern is absolutely valid, and it’s great you’re looking out for your health. Remember to keep hydrated and rest if you start feeling light‑headed, and you’ll be on the right track.
HILDA GONZALEZ SARAVIA
When considering the interaction between phenazopyridine and ethanol, several factors come into play. First, the shared metabolic pathway can delay drug clearance, leading to heightened plasma concentrations. Second, individual variability, such as existing hepatic impairment, can exacerbate these effects. Third, the clinical picture may include dizziness, hypotension, and gastrointestinal upset, which are collectively more troublesome than each symptom alone. Finally, adopting a conservative approach-complete abstinence from alcohol during therapy-offers the safest pathway to recovery.
Carla Taylor
Skip the booze while on the med its simple stay safe and feel better
Kathryn Rude
One must ponder the existential folly of jeopardizing one's physiology for fleeting merriment 😒 The hubris of mixing a targeted analgesic with ethanol betrays a shallow grasp of self‑preservation. It is an act that signals a discord between desire and rationality, a true illustration of Nietzschean decadence. Choose prudence over profane indulgence 🙃
Lindy Hadebe
Simply avoid alcohol with that drug.