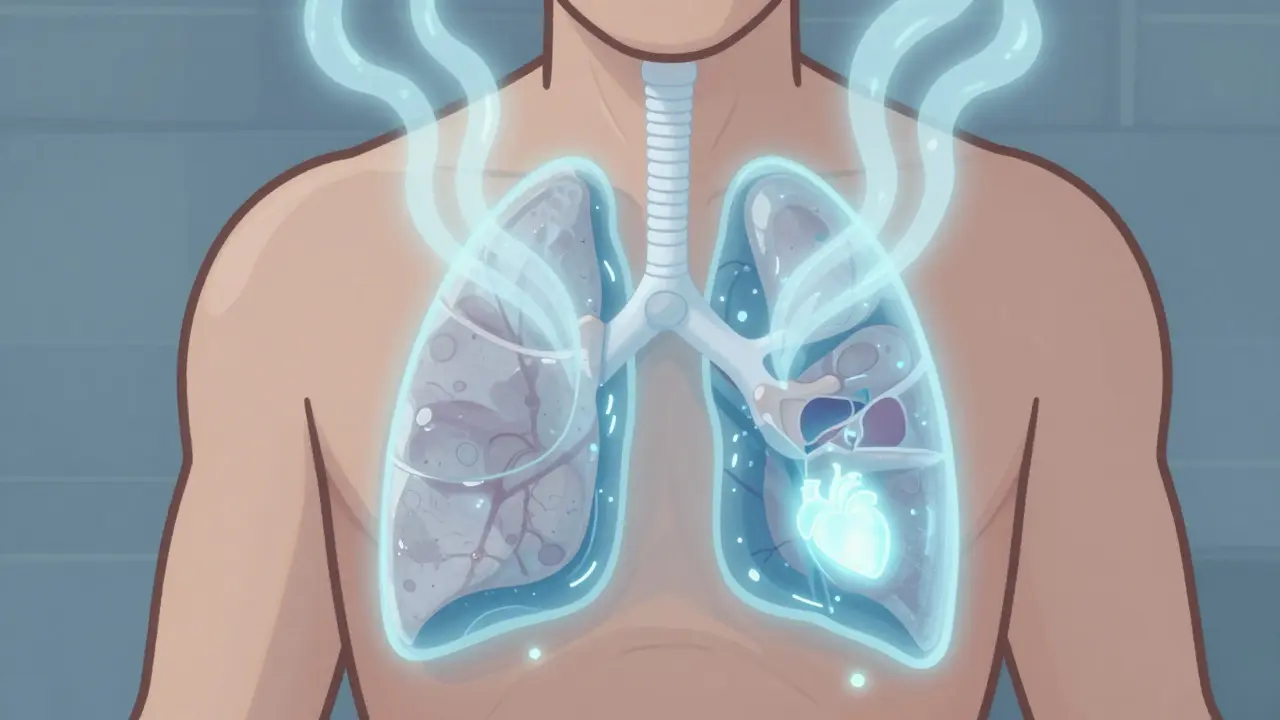
When your lungs can’t expand fully because fluid is building up around them, breathing becomes a struggle. That’s pleural effusion - a condition where excess fluid collects in the space between your lungs and chest wall. It’s not a disease on its own, but a sign something else is wrong. About 1.5 million people in the U.S. deal with it every year. For many, it starts with simple breathlessness. For others, it’s sharp chest pain or a dry cough. The real issue isn’t just the fluid - it’s what’s causing it.
What Causes Pleural Effusion?
Pleural effusions fall into two main types: transudative and exudative. The difference matters because it tells you where to look for the cause.Transudative effusions happen when fluid leaks out because of pressure changes or low protein levels in the blood. The biggest culprit? Congestive heart failure. It accounts for about 50% of all cases, and in transudative cases alone, it’s responsible for 90%. Liver disease like cirrhosis and kidney problems like nephrotic syndrome are other common causes. These aren’t infections or tumors - they’re systemic issues that affect how your body handles fluids.
Exudative effusions are more serious. They’re caused by inflammation, infection, or cancer. Pneumonia is the top cause, making up 40-50% of these cases. Cancer comes next - especially lung, breast, and lymphoma - responsible for 30-40%. Pulmonary embolism and tuberculosis are less common but still important. If your fluid has a low pH, low glucose, or high LDH, it’s a red flag for infection or cancer.
Light’s criteria, developed in 1972, are still the gold standard for telling these apart. If your pleural fluid has a protein-to-serum ratio over 0.5, an LDH-to-serum ratio over 0.6, or LDH more than two-thirds of the upper limit of normal serum LDH - it’s exudative. These rules catch 99.5% of exudative cases. Miss one, and you might miss cancer.
When and How Is Thoracentesis Done?
If you have more than 10mm of fluid on an ultrasound, or if you’re short of breath, doctors will likely recommend thoracentesis. That’s the procedure to drain the fluid - both to help you breathe and to test what’s in it.Ultrasound guidance is no longer optional. It’s the standard. Before ultrasound, complications like a collapsed lung (pneumothorax) happened in nearly 19% of cases. Now? That number is down to 4.1%. That’s an 80% drop in risk. The needle or catheter goes in between your ribs, usually around the 5th to 7th space on your side, just below the armpit. You’re sitting up, leaning forward. It takes minutes.
For diagnosis, they take 50-100 mL - enough to run tests. For relief, they can remove up to 1,500 mL in one session. But removing too much too fast can cause re-expansion pulmonary edema - a rare but dangerous swelling in the lung. That’s why doctors monitor pressure during drainage. If pressure stays under 15 cm H2O, the risk of this complication drops to 5%.
The fluid gets tested for:
- Protein and LDH (to classify as transudate or exudate)
- Cell count and type (white blood cells = infection, red = trauma or cancer)
- pH (below 7.2 means complicated pneumonia or empyema)
- Glucose (below 60 mg/dL suggests infection or rheumatoid arthritis)
- Cytology (to look for cancer cells - found in 60% of malignant cases)
- Amylase (if pancreatitis is suspected)
- Hematocrit (if there’s blood, it could mean pulmonary embolism)
One in four initially undiagnosed effusions turns out to be cancer. That’s why skipping fluid analysis is dangerous.

What Happens After Drainage?
Draining the fluid helps you breathe - but it doesn’t fix the cause. If you have heart failure and don’t treat it, the fluid will come back. If you have cancer and do nothing else, it’ll return even faster.For heart failure patients, the answer is medical management: diuretics, ACE inhibitors, beta-blockers. When doctors use NT-pro-BNP levels to guide treatment, recurrence drops from 40% to under 15% in three months. No surgery needed - just better meds.
For pneumonia-related effusions, antibiotics are key. But if the fluid has a pH below 7.2, glucose below 40 mg/dL, or bacteria on Gram stain, it’s already turning into empyema. Drainage becomes urgent. Without it, 30-40% of these cases become full-blown infections requiring surgery.
After heart surgery, about 15-20% of patients get fluid buildup. Most clear up on their own. But if more than 500 mL drains per day for three days straight, they’ll keep a chest tube in longer - and recurrence drops to 95% prevention.
How to Stop It From Coming Back
The biggest challenge is malignant pleural effusion. Half of these come back within 30 days after just draining the fluid. That’s why long-term solutions are critical.Pleurodesis is the traditional fix. Doctors inject something - usually talc - to make the lung stick to the chest wall. It works in 70-90% of cases. But it’s painful. Up to 80% of patients report moderate to severe pain after the procedure. Hospital stays average 7.2 days.
Now, indwelling pleural catheters (IPCs) are the new standard for cancer patients. These are small tubes left in place for weeks. You drain the fluid at home, usually once a day. Success rates at six months? 85-90%. Hospital stays drop to 2.1 days. Many patients keep the catheter for months or even years. It’s not a cure, but it’s a life-changing way to control symptoms.
The European Respiratory Society now recommends IPCs as first-line for trapped lung from cancer. The American Thoracic Society agrees: don’t use chemical pleurodesis for non-cancer cases - it doesn’t work well and carries risks.
For patients who can’t tolerate surgery or have poor lung function, IPCs are often the only safe option. They’re also better for people who live far from hospitals. No need for repeated trips for drainage.

What You Should Know
The biggest mistake? Treating the fluid without treating the cause. As Dr. Richard Light put it: “It’s like bailing water from a sinking boat without patching the hole.”Ultrasound isn’t a luxury - it’s essential. Every thoracentesis should be guided by it. Every effusion larger than 10mm should be analyzed. And every malignant case needs a plan - not just one-time drainage.
Survival rates for cancer patients with pleural effusion have improved. In 2010, only 10% lived five years. Today, it’s 25%. Why? Better cancer treatments. Better drainage techniques. Better follow-up care.
If you’ve had a pleural effusion, ask: What’s the cause? Was fluid tested? Was ultrasound used? What’s the plan to keep it from coming back? Don’t assume it’s just “fluid on the lung.” It’s your body’s way of screaming for help.
Can pleural effusion go away on its own?
Sometimes, yes - especially if it’s small and caused by heart failure or after surgery. But if it’s due to infection, cancer, or inflammation, it won’t resolve without treatment. Waiting can lead to complications like empyema or trapped lung. Always get it checked.
Is thoracentesis painful?
You’ll feel pressure and a brief sting when the numbing shot is given. During drainage, you might feel a pulling sensation or urge to cough. Most people report mild discomfort, not pain. Ultrasound guidance reduces complications and makes the procedure safer and smoother.
How long does it take to recover after thoracentesis?
Most people feel better right away. You can usually go home the same day. Avoid heavy lifting for 24-48 hours. Watch for signs of infection - fever, redness at the site, or worsening shortness of breath. If you develop sudden chest pain or trouble breathing, seek help immediately - it could be a collapsed lung.
What’s the difference between a pleural effusion and pneumonia?
Pneumonia is an infection inside the lung tissue, causing fever, cough, and mucus. Pleural effusion is fluid outside the lung, in the space between the lung and chest wall. But pneumonia can cause pleural effusion - and if it does, the fluid can become infected (empyema). That’s why fluid analysis is critical: it tells you if the problem is just pneumonia or something worse.
Can pleural effusion be prevented?
You can’t always prevent it, but you can reduce your risk. Manage heart failure with meds and diet. Quit smoking to lower cancer and pneumonia risk. Get vaccinated for flu and pneumonia. If you’ve had one effusion, follow up regularly - recurrence is common, especially with cancer or chronic illness.
Are indwelling pleural catheters safe long-term?
Yes. Studies show they’re safe for months or years. Infection risk is low if you follow home drainage hygiene. Most patients report improved quality of life - less hospital visits, less pain, more control. They’re now recommended as first-line for recurrent malignant effusions, not just as a last resort.
What Comes Next?
If you’ve been diagnosed with pleural effusion, your next steps depend on the cause. For heart failure: optimize meds, track weight daily, limit salt. For pneumonia: finish antibiotics, monitor symptoms. For cancer: talk to your oncologist about indwelling catheters or pleurodesis. Don’t wait for symptoms to return.Ask your doctor: “What’s the exact cause?” “Was ultrasound used?” “What’s the plan to prevent recurrence?” If they don’t have answers, get a second opinion. Pleural effusion isn’t just a fluid problem - it’s a signal. Listen to it.

Meenakshi Jaiswal
Just wanted to say this is one of the clearest explanations I’ve read on pleural effusion. The breakdown between transudative and exudative? Perfect. I’m a nurse in Mumbai and I share this with my students all the time. 🙌
Moses Odumbe
Light’s criteria still rules 👑 1972 called, they want their diagnostic gold standard back. Also, if you’re not using ultrasound? You’re basically playing Russian roulette with a needle. 😅
Monte Pareek
Let me cut through the noise - if you're draining more than 1500ml in one go without monitoring pressure you're asking for re-expansion edema. Period. I've seen it. Patient goes from breathing fine to gasping in 20 minutes. Ultrasound isn't optional. Fluid analysis isn't optional. And IPCs for cancer patients? Not a last resort - it's the smart play. Stop treating symptoms. Treat the damn source. 🚫💧
Connie Zehner
OMG I had this last year and they drained 1.2L and I thought I was gonna die?? But then I found out it was from my lupus and now I’m on biologics and it’s been 8 months no recurrence 😭 thank you for posting this I cried reading it
Tim Goodfellow
Man, I used to think pleural effusion was just ‘water on the lung’ until I watched my dad go through it. Now I see it as the body’s emergency flare - like your car’s check engine light but for your chest. And IPCs? Absolute game-changer. My dad’s been draining at home for 14 months. He’s gardening again. No hospital stays. No pain. Just quiet control. 🌿
Mahammad Muradov
People still use talc pleurodesis? Pathetic. The fact that you’re even considering chemical pleurodesis for non-cancer cases shows how outdated some practices are. IPCs are safer, cheaper, and less painful. If your hospital isn’t offering them, demand a transfer. This isn’t 1995.
holly Sinclair
It’s fascinating how medicine has evolved from treating symptoms as the problem, to recognizing them as signals - metaphors for deeper systemic collapse. The pleural effusion isn’t the disease; it’s the echo of a broken heart, a rogue cell, a leaking vessel whispering in the dark. We drain the fluid, but do we ever truly listen to what it’s saying? The body doesn’t make mistakes. It only responds. And we, in our haste, mistake the response for the cause.
Elaine Douglass
Thank you for writing this. My mom had this after her lung surgery and they didn’t even test the fluid at first. She ended up in the ICU because it turned into empyema. Please please please get it tested. Even if you feel better after draining. It matters.
Vicki Belcher
So proud of how far we’ve come with IPCs! 💪 My cousin has one and she says it’s like having a tiny reset button for her lungs. She laughs now. She travels. She sleeps through the night. It’s not a cure, but it’s a gift. Keep pushing for better care - you’re changing lives. 🌟
bhushan telavane
Here in India, most hospitals still don’t have ultrasound machines for thoracentesis. We use landmarks. It’s scary. But we do what we can. Still, this article gives me hope. Maybe one day every village clinic will have access to this knowledge.
Kelly Mulder
While the data presented is statistically compelling, one must question the epistemological validity of relying solely on Light’s criteria in an era of molecular diagnostics. The reductionist paradigm of fluid analysis, while historically robust, risks overlooking proteomic and cytokine-based biomarkers that may offer superior predictive accuracy. One cannot ethically dismiss emergent paradigms in favor of legacy algorithms.
Takeysha Turnquest
They say the body speaks in whispers until it screams. Pleural effusion? That’s the scream. And we’re still just handing out earplugs instead of turning down the noise. We drain. We patch. We pretend. But the truth? The hole’s still there. And the boat? Still sinking.
Emily P
Can someone explain why NT-proBNP is better than just using BNP for guiding heart failure treatment? I read the paper but didn’t get the difference.