Every year, over 1.3 million medication errors happen in the U.S. - and nearly a quarter of them come from misunderstandings about your prescription label. It’s not just a slip of the pen or a misread number. It’s often something simple: you didn’t ask about the storage instructions, missed the refill limit, or didn’t realize your pill looks different this time. The label is your first line of defense. But if you don’t know what to look for - or what to ask - it’s just a piece of paper. You don’t need to be a doctor to protect yourself. You just need to ask the right questions.
What’s the generic name, and why does it matter?
Pharmacists are required to list both the brand name and generic name on your label. But most people only notice the big, flashy brand name - like Advil - and miss the generic: ibuprofen. Why does this matter? Because if your doctor switches you to a generic version, the pill might look different. Same active ingredient. Same effect. But if you don’t know the generic name, you might think it’s a mistake - or worse, a counterfeit. Always confirm: "Is this the same medicine as before, just under a different name?"
What’s the correct dose, and how often should I take it?
Labels say things like "Take one by mouth every 6 hours as needed for pain." But what does "as needed" really mean? Does it mean every 6 hours even if you’re not in pain? Or only when the pain hits? The FDA requires this info to be clear, but it’s not always. Ask: "Should I take this at fixed times, or only when I feel symptoms?" Also, check the strength. A 5 mg pill is not the same as a 10 mg pill. If you’re switching from one brand to another, or from a liquid to a tablet, confirm the exact dosage. One mistake here can lead to overdose or under-treatment.
What should I avoid taking with this medicine?
Some medications don’t play nice with food, alcohol, or other drugs. For example, statins like atorvastatin can interact with grapefruit juice. Antibiotics like doxycycline lose effectiveness if taken with dairy. Blood thinners like warfarin can become dangerous if mixed with certain supplements. The label might say "avoid alcohol," but it won’t always list every interaction. Ask: "What foods, drinks, vitamins, or over-the-counter meds should I not take with this?" Even something as simple as antacids or calcium supplements can interfere. Your pharmacist has a full drug interaction database - use it.
How should I store this?
Most people assume all pills are fine in the bathroom cabinet. They’re not. According to a 2022 survey, 15% of prescription medications need refrigeration. That includes insulin, certain antibiotics, and even some hormone treatments. If you leave them out, they can lose potency - or worse, break down into harmful substances. Check the label for temperature ranges: "Store at room temperature (68-77°F)" or "Refrigerate (36-46°F)." If it’s not clear, ask: "Does this need to be kept cold?" And if you’re traveling, ask for tips on keeping it safe on the road.
When does this expire, and is it still good?
Expiration dates aren’t just for show. The FDA requires that medications remain effective and safe until that date - if stored properly. But many people keep old pills in drawers for years. If your label says "Exp: 06/2025," that means it’s good until the end of June. After that? No guarantees. Ask: "Is this still safe to use if it’s past the expiration date?" And if you’re refilling a long-term medication, compare the new batch to the old one. If the color, shape, or size changed - even slightly - ask why. It could be a different manufacturer.
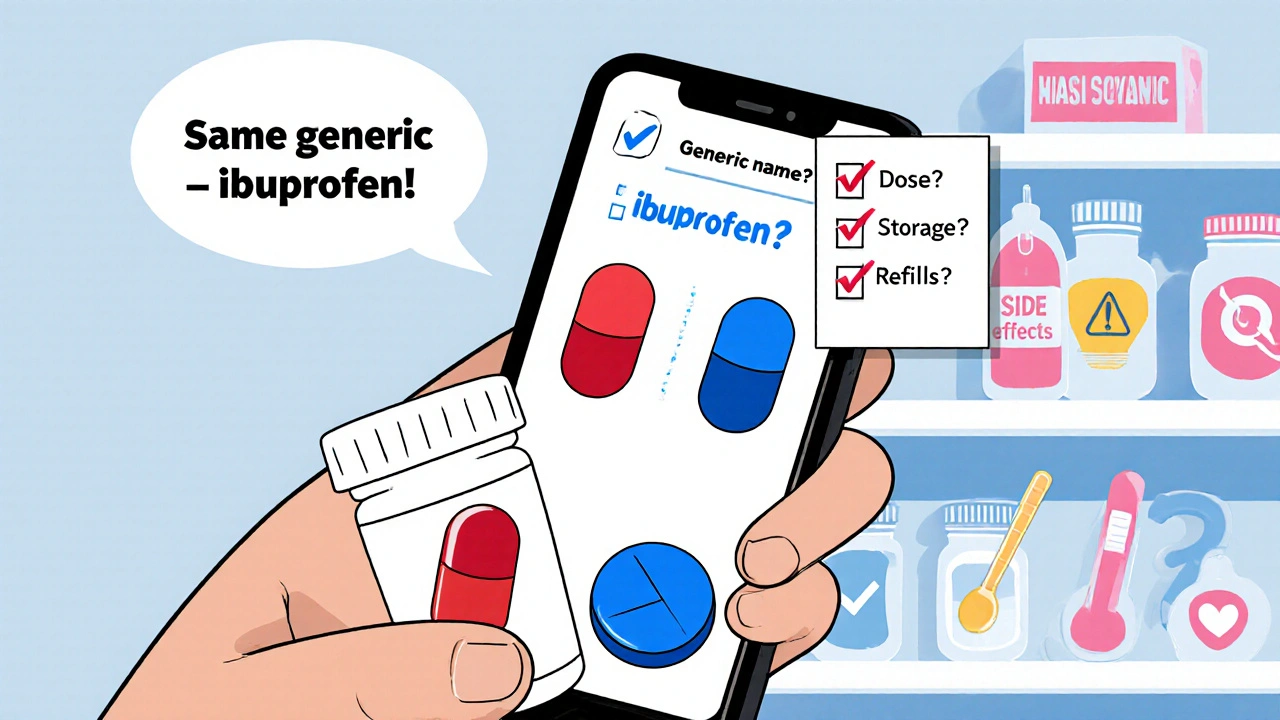
How many refills do I have left?
Pharmacies often print refill info in tiny text at the bottom. You might miss it. Then you show up for your next refill and get a surprise: "No refills left." That’s not just inconvenient - it can be dangerous if you’re on a chronic condition like high blood pressure or diabetes. Always confirm: "How many refills do I have? When will I need a new prescription?" And ask if your doctor can authorize more refills ahead of time. Some states require a new prescription after three refills - even if your doctor meant for you to keep taking it.
What side effects should I watch for?
Labels list side effects - but they’re often buried in fine print. You might see "dizziness, nausea, headache" - but what if you get swelling in your throat, chest pain, or trouble breathing? Those are red flags. Ask: "What are the serious side effects I should call you about right away?" For high-risk drugs like opioids, blood thinners, or diabetes meds, the FDA requires a Medication Guide. If you didn’t get one, ask for it. Don’t assume it’s not important. A 2023 study found that patients who asked about side effects reduced their risk of hospitalization by 34%.
Can you read this back to me?
It sounds simple, but it’s one of the most powerful things you can do. After the pharmacist gives you the label, say: "Can you please read the instructions back to me so I can make sure I got it right?" Then repeat them aloud. This isn’t about doubting the pharmacist - it’s about catching errors. A 2022 report from the American Society of Health-System Pharmacists found that patients who repeated instructions back reduced medication errors by 58%. If the pharmacist hesitates or says, "You don’t need to do that," that’s a red flag. A good pharmacist will welcome it.
Is there a larger-print version or audio help?
Over 7.6 million Americans over 45 have vision problems. Millions more struggle with reading due to low health literacy or learning differences. Pharmacies are legally required to provide accommodations. Ask: "Can I get a large-print label?" or "Do you have a recording or video of these instructions?" Many pharmacies now offer QR codes that link to short videos explaining how to take the medicine. If yours doesn’t, ask if they can print a bigger version. It’s your right. And if English isn’t your first language, ask for a translator. The Affordable Care Act requires it for pharmacies receiving federal funds.

What happens if I miss a dose?
This is one of the most common questions - and one of the most overlooked. If you forget to take your blood pressure pill, should you double up next time? What if you’re on antibiotics? Some drugs are safe to take late. Others can be dangerous. Ask: "If I miss a dose, what should I do?" Don’t guess. Don’t rely on Google. Your pharmacist has the exact protocol for your specific medication.
Why does this look different from last time?
It’s normal for pills to change shape, color, or size - especially if your insurance switched the manufacturer. But if you don’t know why, it’s scary. Always ask: "Is this the same medicine as before? Why does it look different?" If the pharmacist says, "It’s just a different brand," ask for the generic name to confirm. Keep a photo of your pills on your phone. That way, if something looks off next time, you’ll know.
Can I get a written summary?
Pharmacies are required to give you a printed label - but not always a summary. Ask: "Can you give me a one-page cheat sheet of what I need to know?" Include: drug name, dose, timing, storage, key warnings, and who to call. Many independent pharmacies do this automatically. Chain pharmacies might need a nudge. Having this in your wallet or phone makes it easier to show your doctor or emergency responders later.
What’s the next step if something goes wrong?
What if you feel strange after taking the pill? What if you think you took the wrong dose? Ask: "Who do I call if I have a problem after I leave?" Get the pharmacy’s direct line. Some have 24/7 pharmacists on call. Others forward you to an on-call nurse. Don’t wait until you’re in crisis. Know the number now.
Prescription labels aren’t meant to be confusing. But the system isn’t perfect. With over 4.9 billion prescriptions filled each year in the U.S., small mistakes add up fast. The good news? You don’t need to be an expert to fix this. You just need to speak up. Asking five simple questions can cut your risk of a dangerous error by nearly half. Your health isn’t a guessing game. Your label holds the answers. You just have to ask for them.
What should I do if my prescription label looks different from last time?
Always ask the pharmacist: "Is this the same medicine as before? Why does it look different?" Pills can change color, shape, or size because of a different manufacturer - but you need to confirm it’s the same generic drug. Keep a photo of your pills on your phone so you can compare. Never assume it’s a mistake - but don’t take it without verification.
Do I need to refrigerate all my medications?
No. Only about 15% of prescriptions need refrigeration - including insulin, some antibiotics, and hormone treatments. Check the label for storage instructions: "Store at room temperature" or "Refrigerate (36-46°F)." If it’s not clear, ask. Leaving refrigerated meds out can make them ineffective or unsafe. Never store them in the bathroom - heat and moisture ruin most drugs.
Can I take my medication with food?
Some meds need food to reduce stomach upset. Others must be taken on an empty stomach to work properly. For example, doxycycline shouldn’t be taken with dairy - it blocks absorption. Statins work better with a meal. Always ask: "Should I take this with or without food?" The label might say "take with food," but it won’t always explain why. Your pharmacist can tell you the science behind it.
What if I can’t read the label because the print is too small?
You have the right to a large-print label. Over 92% of U.S. pharmacies offer this for free. Ask: "Can you print this in a larger font?" Some pharmacies also offer audio recordings or QR codes that link to video instructions. If you have vision problems or low health literacy, don’t guess - ask for help. It’s your safety, not just a convenience.
How do I know if my prescription has expired?
Look for the expiration date on the label - it’s usually printed in "MM/YYYY" format. If it says "Exp: 06/2025," the medication is safe to use until the end of June 2025. After that, it may lose strength or break down. Never take expired pills for serious conditions like heart disease or infections. If you’re unsure, call the pharmacy. They can check the batch and advise.
Can I refill my prescription early if I’m traveling?
It depends on your insurance and state laws. Most insurers allow early refills for travel - but you need to ask ahead. Call your pharmacy or insurance provider at least a week before your trip. Some states limit early refills to 7 days before the due date. If you’re going abroad, ask if your medication is legal in your destination country. Carry a copy of your prescription in case customs asks.
What if I accidentally take too much?
Call your pharmacy immediately - they can advise you on what to do next. If you’re having symptoms like dizziness, vomiting, chest pain, or confusion, call 911 or go to the ER. Don’t wait. Keep the pill bottle with you when you seek help - it helps medical staff identify the drug and dosage. Many pharmacies have poison control hotlines or 24/7 pharmacist lines. Ask for the number when you pick up your prescription.
Do I need to keep the original bottle?
Yes. The original bottle has the full label with expiration date, lot number, and pharmacy info - all critical in emergencies. Even if you transfer pills to a pill organizer, keep the bottle. If you have a reaction or overdose, first responders need to know exactly what you took. Don’t throw it away until you’re done with the prescription and have no refills left.
Why does my label say "Medication Guide"?
The FDA requires a separate Medication Guide for high-risk drugs - like opioids, blood thinners, or isotretinoin. These guides explain serious side effects in plain language. If you didn’t get one, ask for it. It’s not optional - it’s required by law. These guides can save your life. Don’t skip reading them.
Can I ask the pharmacist to explain everything again?
Absolutely. Pharmacists are trained to explain medications. If you’re unsure, say: "Can you go over this one more time? I want to make sure I understand." Repeat the instructions back to them. Studies show this reduces errors by over 50%. There’s no such thing as asking too many questions. Your safety matters more than their time.


Latrisha M.
Always ask about the generic name. I once took a pill that looked completely different and panicked for days until I checked with my pharmacist. Turns out it was just a generic switch. Knowledge is power.
Jamie Watts
Why do pharmacies even print labels in font size 4? My grandma can't read them and they act like it's her fault. Ask for big print. It's not a favor it's a right. And if they give you grief tell them the ADA has your back.
Teresa Smith
People treat pharmacy labels like they're sacred texts written in ancient Latin. They're not. They're instructions. And like any instruction manual they're only useful if you read them with intent. Don't just glance. Don't assume. Ask the pharmacist to walk you through it. They're paid to explain not just dispense. If you're on multiple meds write them down. Use color coded pill boxes. Create a cheat sheet. Your future self will thank you. Medication errors aren't accidents they're failures of communication. And you're the most important link in that chain.
ZAK SCHADER
Why do we even need to ask these questions anymore? Pharmacies are supposed to be professionals not babysitters. I just take what they give me and move on. If it kills me its their problem not mine.
Danish dan iwan Adventure
Pharmacokinetic variability is often overlooked. Generic substitution may be bioequivalent but not therapeutically equivalent in marginal cases. Always verify AUC and Cmax parameters via pharmacy database.
Ankit Right-hand for this but 2 qty HK 21
Who the hell cares about the label? Big Pharma controls everything anyway. The real issue is why your insurance forces you to switch brands every 3 months. They want you confused so you don't notice the price hikes. Ask for the original prescription. Fight the system.
Oyejobi Olufemi
Why do you think they don't print instructions in bold? Why do you think the expiration date is in the tiniest font? Because they want you to make mistakes. Because they profit from ER visits. Because they're not here to help you. They're here to sell you pills. And if you die? Well that's just another statistic in their quarterly report.
Daniel Stewart
It's interesting how the burden of pharmaceutical literacy falls entirely on the patient. The system is designed for efficiency not safety. One might argue that if the label were truly self-explanatory we wouldn't need 12 questions to decode it.
Deepak Mishra
OMG I JUST REALIZED I’VE BEEN TAKING MY BLOOD PRESSURE MEDS WRONG FOR 3 YEARS!!! 😱 I thought "as needed" meant only when I felt dizzy but now I get it-IT’S A FIXED SCHEDULE!!! I’M SO SCARED BUT ALSO SO GRATEFUL FOR THIS POST!!! 🙏🙏🙏
Diane Tomaszewski
I always ask for a written summary. I keep it in my wallet next to my insurance card. Simple. No drama. Just clear info when I need it.
Dan Angles
It is imperative that patients recognize the legal and ethical obligations incumbent upon pharmacy personnel to provide adequate counseling. Failure to do so constitutes a breach of professional standards under the USP guidelines and may trigger liability under state pharmacy practice acts.
John Mwalwala
Did you know that the FDA allows manufacturers to change pill color and shape without notifying patients? It's part of the Great Medication Switch Program. They do it to track you. Your pills have microchips. The label? It's just a decoy. Always ask for the batch number. Cross-check it with the NSA database. If they refuse? Run.
Rachel Wusowicz
They’re hiding the truth behind the label. The expiration date? It’s a lie. Pills last decades. The real danger is the preservatives they add to make you think they expire. That’s how they keep you buying new ones. I’ve been taking my insulin from 2018. It’s fine. They just want your money.
David Rooksby
Look I get it asking questions is hard and you feel dumb but honestly the whole system is rigged. I had a guy at CVS give me the wrong meds once and when I asked he just shrugged and said 'it's close enough'. I had to go to the manager and threaten to call the state board. They don't want you to ask because then they have to actually do their job. So yeah ask. Ask again. Ask until they roll their eyes. Because if you don't who will? Your doctor? They're busy. Your insurance? They don't care. So you're it. And that's kind of terrifying.