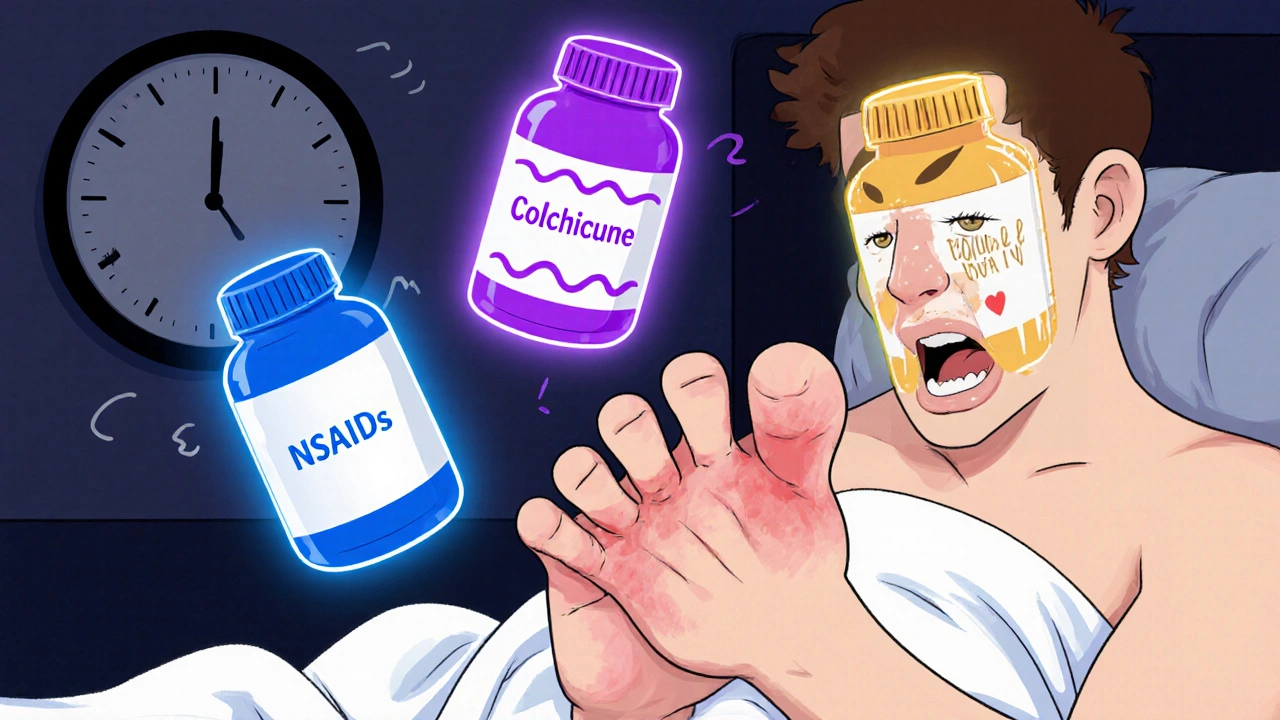
Colchicine vs NSAIDs: Which Is Better for Gout and Inflammation?
When it comes to treating a sudden gout attack, two drugs come up again and again: colchicine, a traditional anti-inflammatory drug specifically used for gout and familial Mediterranean fever. Also known as colchicine sodium, it works by blocking the movement of white blood cells that cause swelling and pain in joints. Then there’s NSAIDs, a broad category of non-steroidal anti-inflammatory drugs like ibuprofen, naproxen, and diclofenac that reduce pain and inflammation by targeting enzymes in the body. Both are used for gout, but they work differently—and one might be safer or more effective for you depending on your health.
Colchicine doesn’t just calm inflammation—it stops the process before it starts. It’s especially useful if you can’t take NSAIDs because of stomach ulcers, kidney problems, or heart issues. But it’s not gentle: nausea, vomiting, and diarrhea are common, especially at higher doses. NSAIDs, on the other hand, work faster and are often easier to tolerate for short-term use. But they can wreck your stomach lining, raise blood pressure, or hurt your kidneys if you take them too long or too often. A 2023 study in the Journal of Rheumatology found that for people over 65 with kidney trouble, colchicine was the safer first choice—NSAIDs increased hospital visits by 37% in that group.
What about cost? Colchicine used to be expensive, but generic versions now cost under $10 a month. NSAIDs like ibuprofen are even cheaper, often under $5. But if you’re taking them daily for arthritis or back pain, the long-term risks add up. For gout flares, you usually only need them for a few days. That’s where colchicine shines: low dose, short course, targeted action. But if you’ve got heart disease or are on blood thinners, NSAIDs might be off-limits. And if you’re on statins, combining them with colchicine can raise the risk of muscle damage. Your doctor needs to know everything you’re taking.
There’s no one-size-fits-all answer. Some people get relief from an NSAID and never need colchicine. Others find colchicine works better, especially if their gout flares are frequent. The key is matching the drug to your body—not just the diagnosis. That’s why the posts below dig into real cases: how people manage side effects, what alternatives exist when one drug fails, and how to talk to your pharmacist about which option makes sense for you. You’ll find comparisons with other pain relievers, tips on avoiding dangerous interactions, and what to do if your current treatment isn’t cutting it. This isn’t theory—it’s what works in real life, for real people.
Gout Flares: Colchicine, NSAIDs, and Steroids Compared
Learn how colchicine, NSAIDs, and steroids compare for treating gout flares. Find out which option is safest and most effective based on your health profile and comorbidities.
More