Gout Steroids: What They Are, How They Work, and What You Need to Know
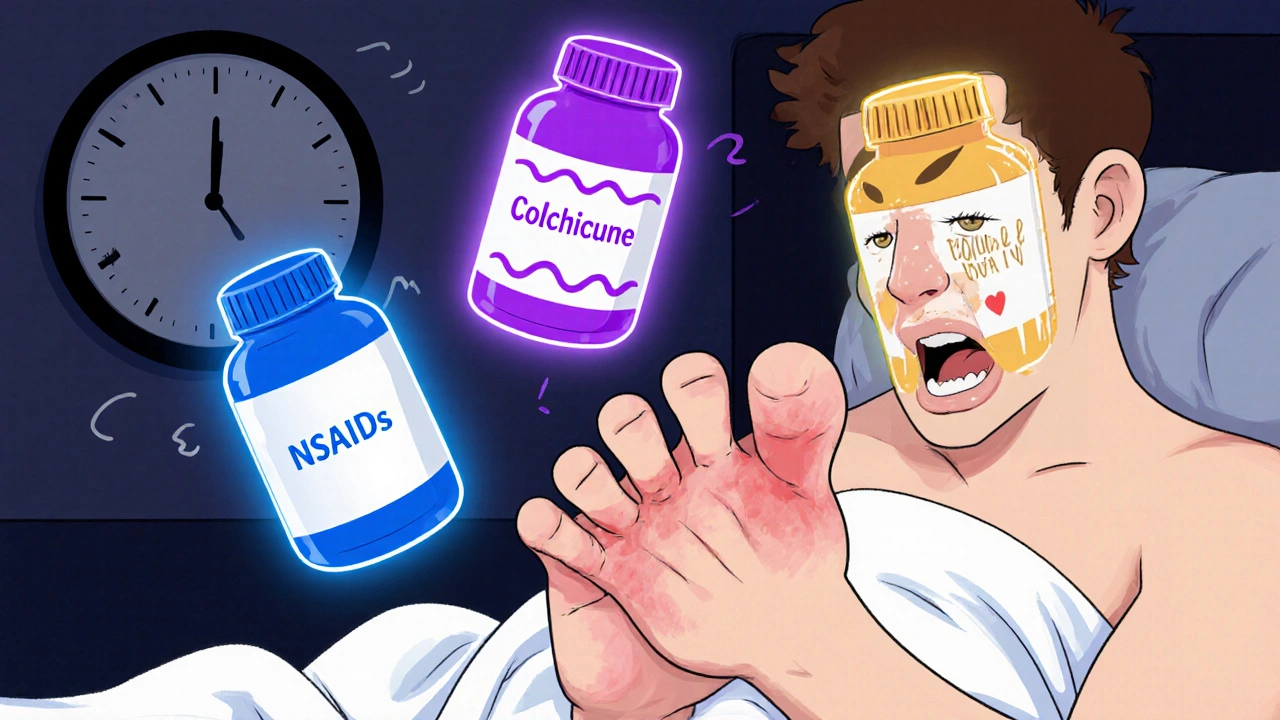
When a gout steroid, a type of corticosteroid used to quickly reduce severe inflammation during a gout flare. Also known as systemic or oral corticosteroids, it works by calming the immune system’s overreaction that causes the intense pain, swelling, and redness in your joints. Gout flares don’t wait for convenience—they hit hard, often at night, and can leave you stuck in bed. That’s where gout steroids come in. Unlike NSAIDs or colchicine, which take time to build up in your system, steroids kick in fast. They’re often the go-to when you can’t take other meds due to kidney issues, stomach ulcers, or if those drugs just aren’t cutting it.
These aren’t your typical daily pills. corticosteroids, hormone-like drugs that mimic natural anti-inflammatory signals in the body like prednisone or methylprednisolone are usually prescribed in short bursts—just a few days to a week. You might start with a higher dose and taper down. This approach avoids long-term side effects like weight gain, bone thinning, or blood sugar spikes. For some, a single injection into the affected joint (like the big toe or knee) works better than pills. It’s targeted, fast, and avoids systemic exposure. But not everyone’s a candidate. If you have diabetes, infections, or osteoporosis, your doctor will weigh the risks carefully.
What makes gout steroids different from other treatments? They don’t lower uric acid levels like allopurinol or febuxostat. Instead, they tackle the inflammation directly. That’s why they’re not for daily use—they’re emergency tools. You’ll still need to manage your long-term uric acid levels, but during a flare, steroids give you breathing room. Many patients report feeling better within 24 to 48 hours. That’s faster than most alternatives.
And while you might hear about NSAIDs, nonsteroidal anti-inflammatory drugs like ibuprofen or naproxen used for pain and swelling as first-line options, they’re not always safe. If you’re on blood thinners, have heart failure, or your kidneys aren’t working well, steroids become the safer bet. Same goes for people who can’t tolerate colchicine’s nausea or diarrhea. In those cases, a short steroid course isn’t just an option—it’s often the best one.
There’s no one-size-fits-all with gout. Some people respond to ice and rest. Others need a combination of meds. But if you’ve been through a bad flare and nothing else worked, steroids are a proven solution. The key is using them the right way: short term, under supervision, and as part of a bigger plan. You’re not just treating pain—you’re protecting your joints from long-term damage.
Below, you’ll find real-world advice from people who’ve been there—how they managed side effects, when they chose steroids over other options, and what their doctors told them to watch for. These aren’t theory pieces. These are experiences from patients and clinicians who’ve seen what works when the pain won’t quit.
Gout Flares: Colchicine, NSAIDs, and Steroids Compared
Learn how colchicine, NSAIDs, and steroids compare for treating gout flares. Find out which option is safest and most effective based on your health profile and comorbidities.
More