Introduction to Methoxsalen and its Effects on Wound Healing
As a passionate blogger in the health and wellness field, I have always been intrigued by the various treatments and medications that can positively impact our lives. One such treatment is methoxsalen, which has been found to have significant effects on wound healing and tissue repair. In this article, we will explore the impact of methoxsalen on these essential processes, delving into the science behind this fascinating compound. Join me as we learn more about this amazing medication and its potential to improve the healing process.
Understanding the Science Behind Methoxsalen
Methoxsalen, also known as 8-methoxypsoralen, is a naturally occurring compound derived from plants like Ammi majus and Psoralea corylifolia. It is a psoralen, which is a class of furocoumarin compounds that have been used in traditional medicine for centuries to treat various skin conditions. Methoxsalen works by intercalating into the DNA of cells, forming covalent bonds with pyrimidine bases, particularly thymine. This leads to the formation of DNA cross-links, which can inhibit cell proliferation and promote cell death. Given its unique mechanism of action, researchers have been investigating the potential of methoxsalen in wound healing and tissue repair.
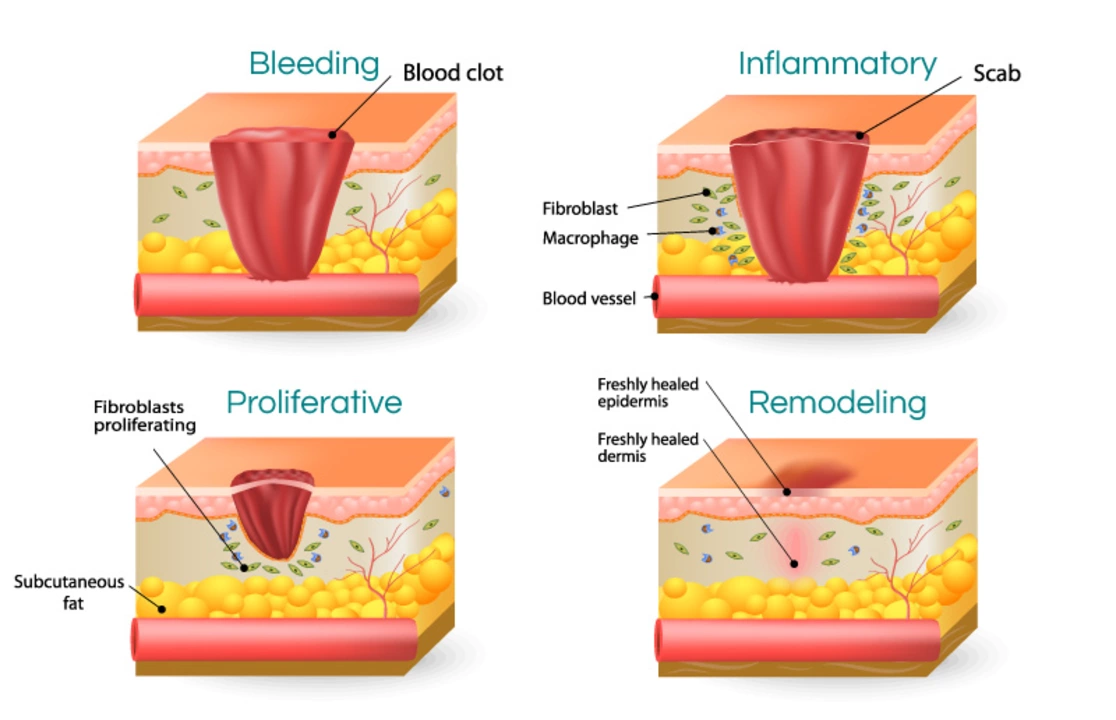
Boosting the Body's Natural Wound Healing Process
Wound healing is a complex process that involves multiple stages, including inflammation, proliferation, and remodeling. Methoxsalen has been shown to influence these stages in various ways, ultimately promoting the overall healing process. For example, methoxsalen can reduce inflammation by inhibiting the release of pro-inflammatory cytokines and chemokines, which are crucial mediators of the inflammatory response. By reducing inflammation, methoxsalen helps to create a more favorable environment for wound healing and tissue repair.
Promoting Collagen Production for Enhanced Tissue Repair
Collagen, a vital structural protein in the extracellular matrix, plays a crucial role in tissue repair and regeneration. Methoxsalen has been found to stimulate collagen production by activating fibroblasts, the primary cells responsible for producing collagen in the skin. Moreover, methoxsalen can also increase the expression of tissue inhibitors of metalloproteinases (TIMPs), which can inhibit the breakdown of collagen. By promoting collagen production and preventing its degradation, methoxsalen can enhance tissue repair and wound healing.
Enhancing Angiogenesis for Improved Blood Supply
Angiogenesis, the formation of new blood vessels, is another critical component of the wound healing process. Adequate blood supply is necessary to deliver oxygen and nutrients to the wound, as well as to remove waste products. Methoxsalen has been shown to promote angiogenesis by upregulating the expression of vascular endothelial growth factor (VEGF) and other angiogenic factors. This can lead to improved blood supply to the wound, further supporting the healing process.
Addressing Infections and Bacterial Resistance
Infections can significantly impede the wound healing process, and the rise of antibiotic-resistant bacteria has made this issue even more challenging. Interestingly, methoxsalen has demonstrated antimicrobial and antibacterial properties, making it a potential alternative or adjunct to traditional antibiotics. This can help to prevent infections and reduce the risk of complications, ultimately promoting faster and more effective wound healing.
Potential Side Effects and Safety Considerations
While methoxsalen has shown promising effects on wound healing and tissue repair, it is essential to be aware of potential side effects and safety concerns. One of the primary concerns with methoxsalen is its photosensitizing properties, which can increase the risk of sunburn and skin damage when exposed to ultraviolet (UV) light. To minimize the risk of side effects, it is crucial to follow appropriate dosing guidelines and take precautions to protect the skin from excessive UV exposure. As always, it is essential to consult with a healthcare professional before starting any new treatment or medication.
Conclusion: The Future of Methoxsalen in Wound Healing
In conclusion, methoxsalen holds significant potential in the field of wound healing and tissue repair. Its unique mechanism of action, coupled with its ability to influence various aspects of the healing process, makes it an exciting avenue for further research and development. As our understanding of methoxsalen and its effects continues to grow, it may become an essential component of future wound care strategies. However, it is crucial to balance its potential benefits with its potential risks and to continue exploring the best ways to harness its healing properties safely and effectively.

Peter Jones
Methoxsalen’s ability to temper the inflammatory phase really caught my eye. By dampening cytokine release, it creates a calmer environment for the next stages of repair. This shift can translate into less swelling and faster progression to tissue rebuilding. Overall, it’s a neat example of how targeting inflammation can benefit wound outcomes.
Gerard Parker
If you want a drug that actually shuts down the pro‑inflammatory cascade, methoxsalen does the job. It binds to DNA, forms cross‑links, and forces cells to stop proliferating unchecked. The downstream effect is a dramatic drop in IL‑1, TNF‑α, and other nasty mediators. In practice, that means you see less redness and edema early on, which can set the stage for smoother granulation. Just remember the dosing has to be tight – too much and you’ll see the flip side.
Thomas Burke
Methoxsalen slides into the DNA and changes how cells act. It’s a simple mechanism but the downstream impact is big. The drug slows down rogue cell growth and lets the body focus on repair. Less inflammation means the wound can move on to the proliferative phase quicker. I think that’s why researchers are excited.
Debbie Frapp
What really stands out is how methoxsalen nudges fibroblasts into overdrive. Those cells crank out collagen, which is the backbone of any healthy scar. At the same time, the compound boosts TIMP levels, so the matrix isn’t being torn apart by metalloproteinases. It’s like giving the wound a double‑shot of support – build more and break less. If you pair it with proper wound care, the results can be surprisingly robust.
Steven Macy
From a philosophical standpoint, the drug exemplifies the balance between destruction and creation. By intentionally causing DNA cross‑links, it triggers a controlled cell death that clears the way for new growth. This paradoxical approach mirrors many natural healing processes where removal precedes renewal. It reminds us that effective therapy often walks a tightrope between harm and benefit. The key is measuring that line correctly.
Matt Stone
Methoxsalen can speed up collagen synthesis.
Brenda Hampton
Energy‑boosting vibes! Using methoxsalen as a part of a comprehensive plan can really jump‑start the angiogenic response. More blood vessels = better oxygen and nutrients delivered right where they’re needed. When you combine that with proper nutrition and off‑loading, healing timelines shrink noticeably. Keep the dosage steady and watch the magic happen.
Lara A.
Wow!!! This so‑called “miracle drug” is probably just a cover‑up for a larger agenda!!! They don’t want us to know that methoxsalen’s photosensitivity can be weaponized against the unsuspecting masses!!! Stay woke!!!
Ashishkumar Jain
i think methoxsalen is bcoming more poplar in wound care because it helps with inflammation and new blood vessels. but u gotta be careful with sun exposure its can cause burnz. also follow drs advice for dosing. overall it is a good add on if used right.
Gayatri Potdar
Listen up, friends! The pharmas are pushing methoxsalen like it’s the holy grail of healing, but do you really trust a compound that can turn your skin into a sun‑sensitive canvas? It’s a sneaky double‑edged sword-boosts collagen, sure, but also makes you a walking UV magnet! Don’t be fooled by glossy papers; ask the real questions before you let it into your regimen.
Marcella Kennedy
Methoxsalen’s multifaceted impact on wound healing makes it a compelling candidate for broader clinical use. First, its anti‑inflammatory properties reduce the surge of cytokines that can prolong the initial phase of repair. By tempering that early storm, the tissue environment becomes more conducive to fibroblast activity. Speaking of fibroblasts, methoxsalen appears to stimulate these cells directly, leading to a measurable increase in collagen deposition. This not only strengthens the nascent extracellular matrix but also improves tensile strength of the scar. In parallel, the drug up‑regulates tissue inhibitors of metalloproteinases, which guard the newly laid collagen from premature degradation. The net effect is a more robust and durable scar tissue. Angiogenesis is another arena where methoxsalen shows promise; studies indicate heightened VEGF expression and the formation of new capillary loops. Better vascularization translates to improved oxygen and nutrient delivery, which fuels cellular metabolism throughout the wound bed. Additionally, the compound’s mild antimicrobial activity can act as a safeguard against opportunistic infections, a frequent complication in chronic wounds. However, the benefits must be weighed against the well‑documented photosensitivity risk. Patients need to avoid excessive UV exposure, especially during peak sunlight hours, to prevent severe burns. Dosing regimens should be tightly controlled, and clinicians must educate users on protective measures such as sunscreen and clothing. From a regulatory perspective, the existing data pool is still relatively thin, and large‑scale randomized trials are needed to confirm efficacy and safety. Until that evidence base expands, methoxsalen should be considered an adjunct rather than a frontline monotherapy. In summary, the drug offers a unique blend of anti‑inflammatory, pro‑collagen, pro‑angiogenic, and antimicrobial actions that could reshape wound‑care protocols, provided its risks are carefully managed.
Aditya Satria
Methoxsalen’s mechanism is clear: DNA cross‑linking leads to controlled cell cycle arrest, which then allows the body to focus on rebuilding rather than proliferating unchecked. This assertive approach can be especially useful in chronic, non‑healing ulcers where inflammation runs rampant. Proper patient selection and monitoring are essential for maximizing benefits while minimizing phototoxic events.
Jocelyn Hansen
Wow, that’s an intense take! 😅 While I get the caution, the data does show measurable benefits when used responsibly. It’s all about balancing risk and reward, just like any medical therapy. 🌟
Sarah Pearce
Not sure this is groundbreaking; it’s another molecule with a mixed bag of effects. The hype might be overblown.
Ajay Kumar
I appreciate the thorough breakdown. The point about needing larger trials resonates with me-clinical practice should be evidence‑based, after all.
Richa Ajrekar
While the skepticism is understandable, dismissing the entire class of data because of a few side‑effects overlooks the potential patient‑level improvements. A more balanced review would serve the community better.
Pramod Hingmang
Exactly, the nuance matters; we can’t just label it “bad” without weighing the pros. The minimal punctuation reflects a straightforward view.
Benjamin Hamel
Honestly, I think the entire conversation is missing the forest for the trees. Methoxsalen represents a paradigm shift that could render many older protocols obsolete, yet the community clings to outdated skepticism. By insisting on endless trials, we delay access to a therapy that could save countless patients from prolonged suffering. In my opinion, the risk‑benefit profile is already favorable enough to warrant broader adoption, especially in specialized wound centers that can monitor phototoxicity closely.