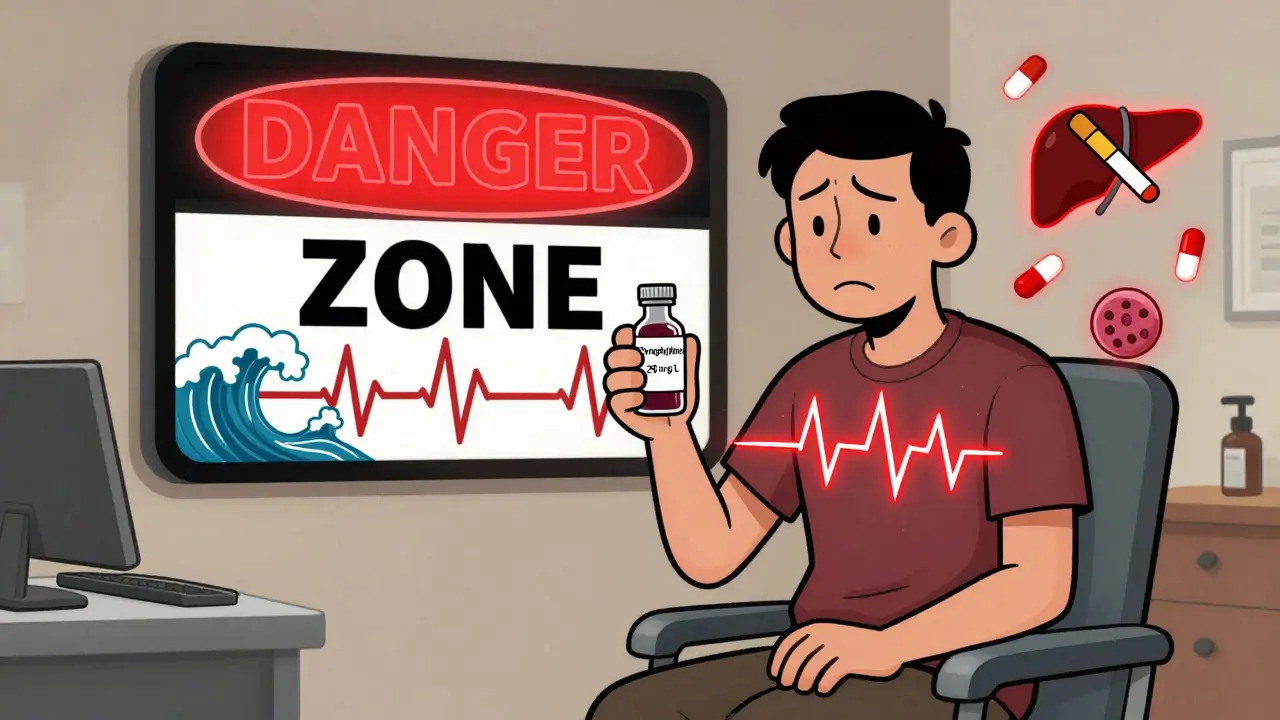
When a drug works only within a tiny window between helping you and hurting you, you don’t just hope it’s working-you check. That’s the reality with theophylline, a decades-old bronchodilator still used for severe asthma and COPD. Its therapeutic range? Just 10 to 20 mg/L. Go below that, and it barely opens your airways. Go above it, and you risk seizures, irregular heartbeats, or even death. This isn’t theoretical. Every year, over 1,500 people in the U.S. end up in the emergency room because their theophylline level crept too high-and about 10% of those cases are fatal.
Why theophylline is so dangerous to get wrong
Theophylline isn’t like insulin or blood pressure meds where you can adjust the dose and wait a few days to see the effect. It’s unpredictable. Two people can take the same 400 mg dose, and one might have a level of 12 mg/L while the other hits 28 mg/L. Why? Because how your body breaks down theophylline depends on a dozen factors you can’t control. Smoking? It speeds up metabolism by 50-70%. That means smokers often need higher doses. But if they quit, their levels can spike dangerously within days. Liver disease? That cuts clearance by half. Heart failure? Same thing. Pregnancy? Levels drop 30-50% in the third trimester. Even something as simple as drinking alcohol can lower theophylline concentration. And then there are the drug interactions. Antibiotics like clarithromycin or ciprofloxacin can double your theophylline level. Antiseizure drugs like carbamazepine can slash it by 60%. One prescription change, and you’re in the danger zone.How monitoring works-and why timing matters
You can’t just check theophylline levels anytime. Timing is everything. For immediate-release tablets, blood must be drawn right before your next dose-that’s the trough level, the lowest point in your cycle. For extended-release versions, you need to wait 4 to 6 hours after taking it. Draw it too early, and you think the dose is too low. Too late, and you think it’s too high. Either way, you make the wrong call. Initial monitoring happens 5 days after starting the drug-or 3 days after any dose change. That’s how long it takes for the drug to reach steady state in your blood. After that, stable patients get checked every 6 to 12 months. But if you’re over 60, have heart or liver problems, or are pregnant? You’re getting tested every 1 to 3 months. Monthly during pregnancy. No exceptions.What happens when levels go off track
A level of 20 mg/L is the upper limit. At 25 mg/L, nausea and tremors become common. At 30 mg/L, you’re looking at seizures and life-threatening arrhythmias. A 2023 case report described a 68-year-old man with COPD who started taking ciprofloxacin for a sinus infection. Three days later, his theophylline level jumped from 14 mg/L to 28 mg/L. He developed ventricular tachycardia. He nearly died. But it’s not just about high levels. Low levels mean the drug isn’t working. Patients with asthma or COPD who don’t get enough theophylline continue to wheeze, flare up, and end up in the hospital. One study found that when clinics started using a standardized monitoring protocol, adverse events dropped by 78%. Asthma control scores improved by 35%. That’s not a small win-it’s life-changing.
What else you need to monitor besides blood levels
Checking theophylline concentration isn’t enough. You need to look at the whole picture. Is the patient’s heart rate above 100 beats per minute? That’s a red flag. Are they jittery, having headaches, or can’t sleep? Those are early signs of toxicity. Are their potassium levels low? That’s common in asthma patients on steroids or albuterol-and low potassium makes arrhythmias more likely. You also need to watch for bone marrow suppression, though it’s rare with modern dosing. And if someone’s getting IV theophylline? Never mix it with dextrose solutions. It can cause clumping or hemolysis. That’s not just a technical note-it’s a safety rule.Why some doctors still use it-and why they can’t stop monitoring
You might wonder: why use theophylline at all? Newer inhalers and biologics are safer, right? Yes. But they cost $200 to $400 a month. Theophylline? $15 to $30. In low-resource settings, it’s the only option. Even in the U.S., it’s still prescribed as a third-line treatment for patients who don’t respond to high-dose steroids and long-acting bronchodilators. Some argue that low doses (200 mg/day) are safe enough to skip monitoring. But the European Respiratory Society and the American College of Chest Physicians say no. Even at low doses, metabolism can change overnight due to illness, new meds, or aging. One study found that 22% of theophylline-related emergencies were caused by unmonitored antibiotic interactions. That’s not a fluke-it’s a pattern.

Husain Atther
Theophylline is one of those drugs that reminds you medicine isn't just about science-it's about patience, vigilance, and listening. I've seen patients on it for years, and the ones who thrive are the ones who treat their blood levels like a monthly check-in with their own body. Not a chore. A ritual.
Izzy Hadala
While the therapeutic window is indeed narrow, the pharmacokinetic variability of theophylline is compounded by interindividual differences in CYP1A2 enzyme activity, which is influenced by genetic polymorphisms, environmental inducers, and concomitant medications. The data presented here aligns with current ACCP guidelines, yet clinical adherence remains suboptimal in community settings due to resource constraints and provider complacency.
Marlon Mentolaroc
Bro. Theophylline is basically the wild west of asthma meds. One day you're chillin', next day you're in the ER because your cousin gave you a bottle of cough syrup with dextromethorphan and now your heart's doing the cha-cha. I've seen it. It's not a joke. And yeah, it's $15. But your life? Priceless. Stop treating it like aspirin.
Gina Beard
Control is an illusion. We measure levels like we're measuring the wind. But the truth is, the body never stops changing. And the drug just waits. Patient. Silent. Waiting for the moment you forget.
Don Foster
Anyone who thinks you can skip monitoring on low dose is either a med student who just read the abstract or a doctor who stopped reading journals in 2008. The ERS and ACCP don't say 'maybe' they say 'DO NOT'. End of story. Also why is everyone still using this when we have biologics? Oh right money. Always money.
siva lingam
So we're still doing blood tests for a $15 pill in 2025? Cool. I'll just keep my asthma in a jar and wave at it.
Shelby Marcel
wait so if you smoke and then quit your theophylline can just… spike?? like overnight?? that’s wild. i had no idea. my uncle did that and thought he was having a panic attack. turns out it was the drug. yikes.
blackbelt security
Every time I see a patient on theophylline, I remind them: you're not just taking a pill. You're part of a system. Your body. Your doctor. Your lab. Your honesty. Miss one link, and the whole chain breaks. Stay sharp. You've got this.
Josh McEvoy
my cousin took theophylline and ended up in the hospital with a heart rate of 180… and then his doctor blamed him for ‘not following instructions’… like he knew his meds would react with his new Zpack?? 😭💀 #TheophyllineIsATickingTimeBomb
Heather McCubbin
It's not about the drug. It's about how we treat people who need it. We give them a pill with a death sentence written in microtext and expect them to be perfect. We don't even give them a pamphlet. Just a lab slip and a prayer. That's not medicine. That's negligence dressed in white coats
Tiffany Wagner
I've been on it for 8 years. Blood tests are annoying but I'd rather do them than end up in the ICU. My last level was 15.5. Felt like a victory.
Chloe Hadland
Thank you for writing this. My mom’s on theophylline and I never understood why she had to get blood drawn so often. Now I get it. I’ll help her keep track of her meds and tell her doctor if she starts any new supplements. She deserves to breathe easy.
Amelia Williams
Just had a patient on theophylline who quit smoking 10 days ago and didn't tell his doctor. Level went from 12 to 27. He had a seizure on the way to the hospital. I’m still shaken. This isn’t just a lab number. It’s a heartbeat. A breath. A life. Please. Tell your doctor everything. Even the small stuff. Even the embarrassing stuff. Your life depends on it.