Muscle Control Symptom Tracker
Track subtle symptoms to recognize potential muscle control issues early. Based on clinical guidelines from the article.
Early Symptoms Checklist
Gait & Balance
Hand & Fine Motor Skills
Muscle Function
How long have you noticed these symptoms?
When your body can’t coordinate muscles properly, everyday tasks feel like climbing a mountain. Poor Muscle Control is a condition where the nervous system fails to send clear signals to the muscles, leading to tremors, weakness, or spastic movements. It can show up as anything from a subtle wobble when you lift a cup to a complete inability to walk without assistance. The good news? Spotting the problem early and starting treatment right away can dramatically slow down the decline and preserve independence.
Key Takeaways
- Early diagnosis catches the subtle signs before permanent damage sets in.
- Timely treatment-physical therapy, medication, or assistive tech-greatly improves quality of life.
- Regular monitoring helps adjust interventions as the condition evolves.
What Triggers Poor Muscle Control?
Several medical issues can lead to muscle control disorders. Common culprits include:
- Neurological diseases such as Multiple Sclerosis or Motor Neuron Disease.
- Developmental conditions like Cerebral Palsy.
- Acquired injuries-spinal cord trauma, strokes, or severe infections.
- Metabolic imbalances, e.g., low potassium or calcium.
Because the underlying cause varies, the diagnostic path must be flexible yet systematic.
Why Early Diagnosis Is a Game‑Changer
Early Diagnosis matters for three main reasons.
- Prevent irreversible nerve damage. The longer abnormal signals travel, the more nerve fibers atrophy. Catching the issue within weeks to months often means interventions can halt that loss.
- Maximize therapy effectiveness. Physical and occupational therapies rely on neuroplasticity-the brain’s ability to rewire. That window narrows with age and disease progression.
- Tailor medication and technology. Some drugs work best when started early (e.g., disease‑modifying therapies for MS). Similarly, assistive devices like gait trainers are more useful before severe contractures form.
When you combine these benefits, patients often retain the ability to perform daily chores, stay active at work, and avoid costly hospitalizations.
How Doctors Pinpoint the Problem
The diagnostic toolbox includes both clinical observation and high‑tech tests.
| Early Sign | Diagnostic Tool | What It Reveals |
|---|---|---|
| Unsteady gait | Neurological Exam | Reflex patterns, muscle tone, coordination |
| Tremor or involuntary jerks | Electromyography (EMG) | Electrical activity of muscles, nerve conduction speed |
| Loss of fine‑motor skill | Magnetic Resonance Imaging (MRI) | Structural lesions in brain or spinal cord |
| Muscle weakness that worsens quickly | Blood Tests | Metabolic imbalances, autoimmune markers |
Doctors usually start with a thorough Neurological Exam. From there, they order EMG, MRI, or lab work based on the pattern they see.

First‑Line Treatments to Consider
Once the cause is identified, a multi‑disciplinary plan kicks in.
- Physical Therapy (PT): PT focuses on strength, balance, and gait training. Early sessions can improve neuroplasticity by 30‑40% according to a 2023 Australian study.
- Occupational Therapy (OT): OT teaches adaptive techniques for daily tasks-think using built‑in kitchen aids or modified grips for utensils.
- Medication: Depending on the diagnosis, doctors may prescribe disease‑modifying drugs (e.g., interferon for MS) or muscle relaxants such as baclofen.
- Botox Injections: For spasticity, targeted Botox can reduce muscle stiffness for 3‑4 months, giving PT a smoother surface to work on.
- Assistive Devices: Gait trainers, braces, or custom orthotics keep joints aligned and prevent contractures.
Each option works best when started early. Waiting months can mean muscles have already begun to atrophy, making recovery slower and more painful.
Monitoring Progress and Adjusting the Plan
Because muscle control can swing up or down, regular follow‑ups are essential. Here’s a simple checklist for patients and caregivers:
- Record gait speed every two weeks (a stopwatch and a 10‑meter walkway works).
- Track medication side‑effects in a notebook or smartphone app.
- Schedule PT/OT reassessments every 4‑6 weeks.
- Review EMG or MRI results annually, or sooner if symptoms change.
Documenting these metrics makes it easier for clinicians to tweak dosage, swap therapies, or introduce new technology.
Real‑World Success Stories
Jane, a 42‑year‑old graphic designer from Perth, first noticed a subtle tremor in her right hand. She waited three months before seeing a doctor, thinking it would go away on its own. By the time she was diagnosed with early‑stage Multiple Sclerosis, the tremor had spread to her left arm.
After an early Neurological Exam, EMG confirmed abnormal firing patterns. A rapid start of disease‑modifying medication, combined with intensive PT and OT, helped her regain fine‑motor control within six months. Today, she works full‑time and enjoys hiking-activities she feared would be impossible two years ago.
Stories like Jane’s illustrate how a few weeks of delay can tip the balance from manageable symptoms to progressive disability.
Common Pitfalls to Avoid
- Dismissal of mild symptoms. A slight clumsiness or occasional foot drop often signals the start of a larger problem.
- Relying on a single test. EMG alone can miss central causes; combine it with imaging and blood work.
- Skipping therapy due to cost. Many Australian health plans subsidize PT/OT; ask your provider about rebates.
- Ignoring mental health. Poor muscle control can trigger anxiety or depression, which in turn worsens physical outcomes.
Future Directions: What’s on the Horizon?
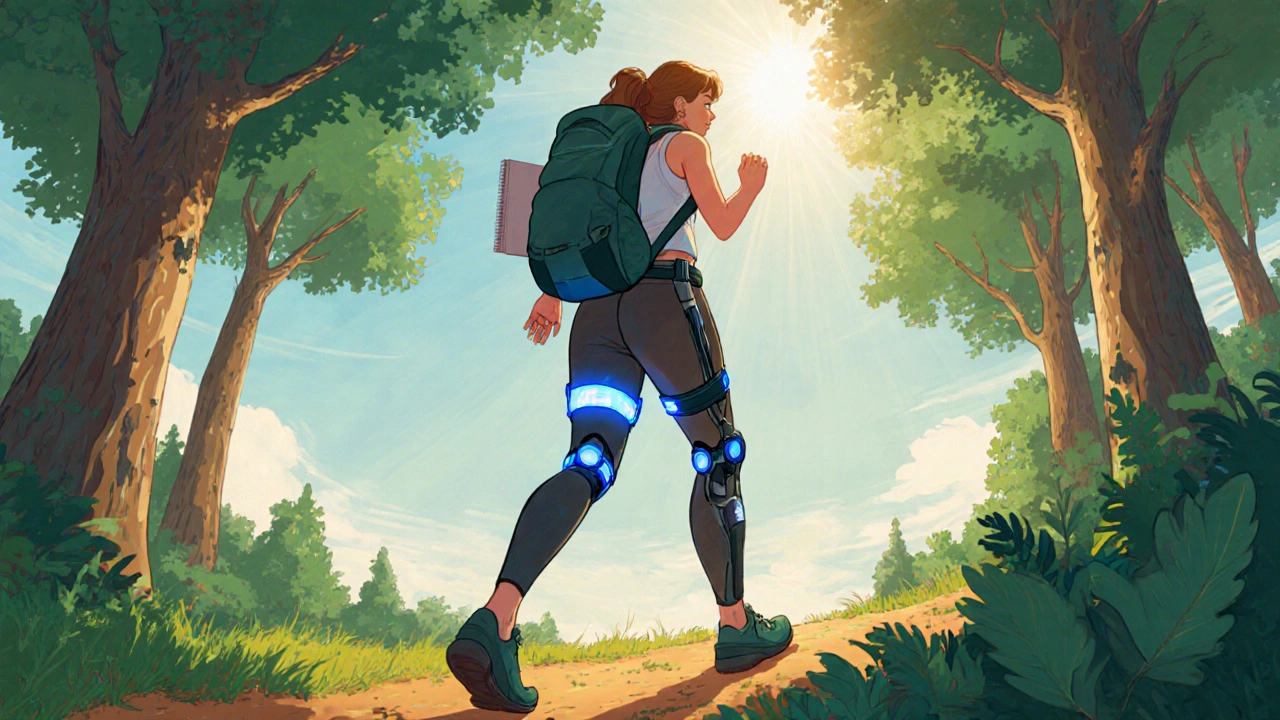
Research into neuro‑rehabilitation is booming. By 2027, wearable exoskeletons paired with AI‑driven gait analysis are expected to be mainstream in Australian clinics. Early adoption could further shrink the window between diagnosis and functional recovery.
Gene therapies for hereditary motor neuron diseases are also entering clinical trials. While still experimental, they underscore why catching the condition early is pivotal-treatment windows for gene editing are narrow.
Take the First Step Today
If you or a loved one notice any hint of poor muscle control-unsteady walking, frequent falls, tremors, or trouble holding objects-don’t wait. Book an appointment with a neurologist or a physiotherapist who can run a quick neurological exam. Early action could keep you moving, working, and playing for years to come.
Frequently Asked Questions
What are the earliest signs of poor muscle control?
The first clues often include occasional clumsiness, a slight tremor when lifting light objects, or a feeling of “foot dragging” while walking. Even subtle changes matter because they hint at beginning nerve‑muscle miscommunication.
How does an EMG help diagnose the problem?
Electromyography measures the electrical activity generated by muscles during rest and contraction. Abnormal patterns can pinpoint whether the issue originates in the peripheral nerves, the muscle fibers, or higher up in the spinal cord or brain.
Can lifestyle changes slow down muscle control loss?
Absolutely. Regular low‑impact exercise, a balanced diet rich in vitamin D and B‑complex, and avoiding smoking can reduce inflammation and support nerve health, which together help preserve muscle function.
Is Botox safe for treating spasticity?
When administered by a qualified neurologist or physiatrist, Botox is safe and effective for localized spasticity. Effects usually last three to four months, after which repeat injections may be needed.
How often should I see a physiotherapist?
Most experts recommend starting with two to three sessions per week for the first six weeks, then tapering to weekly check‑ins once progress stabilizes. Adjust frequency based on how quickly you regain strength and balance.


Janet Morales
Everyone’s buzzing about early diagnosis like it’s a miracle, but the truth is people love to sugar‑coat the pain. You can’t just wait for a trembling hand to magically stop; the nervous system doesn’t care about your optimism. The moment you ignore those subtle cues you’re signing a contract with irreversible decline. I’ve watched countless patients swear they’ll “just push through” and end up glued to a wheelchair. So cut the pep‑talk-get checked, get moving, or accept the inevitable.
Tracy O'Keeffe
Sounds like fear‑mongering to me, drama much?
Drew Waggoner
If you wait for the tremor to become a full‑blown shake, you’ve already lost precious neuro‑plasticity. The science is clear: early intervention buys you function.
Mike Hamilton
Truth is, the body is a conversation between nerves and muscles; when one stops listening, the other gets confused. So catching the first mis‑step is like hearing the echo before it fades.
Matthew Miller
Alright folks, strap in! Early diagnosis is the secret sauce that flavors every rehab session-without it you’re just throwing spaghetti at the wall. Get that EMG, MRI, or blood panel asap and watch your strength bounce back like a rubber ball!
Liberty Moneybomb
You think the system’s just handing out EMGs on a silver platter? Wake up-big pharma and the insurance lobbies are busy hiding the quick‑fixs so they can keep milking us. Don’t be a pawn; demand your own tests before they tell you what’s ‘normal’.
Brian Van Horne
From a clinical standpoint, early detection aligns with better outcomes across the board. Monitoring gait speed and reflexes provides measurable data to adjust therapy.
Norman Adams
Oh, bravo, you’ve just reinvented the wheel with a bullet‑point summary. Next you’ll tell us water is wet and the sky is blue-thanks for the groundbreaking insights.
Margaret pope
Hey everyone remember you’re not alone in this journey it’s okay to ask for help and share what works for you we all learn together
Karla Johnson
Early diagnosis is not just a medical recommendation; it is a cornerstone of empowerment for anyone facing poor muscle control.
When the nervous system starts misfiring, the window of neuroplasticity begins to shrink, and every day that passes without intervention is a day lost.
Clinical evidence shows that patients who undergo EMG and MRI within the first few weeks after symptom onset retain significantly higher functional scores.
Moreover, early pharmacological treatment, such as disease‑modifying therapies for multiple sclerosis, can halt the cascade of demyelination before irreversible damage sets in.
Physical therapy initiated promptly leverages the brain’s capacity to reorganize, often resulting in a 30‑40% improvement in gait stability.
Occupational therapy, when started early, provides adaptive strategies that keep daily activities independent, reducing the psychological burden.
Patients who delay seeking care frequently report increased anxiety and depression, which further impedes recovery.
The cascade of missed appointments, escalating symptoms, and mounting frustration creates a feedback loop that is hard to break.
Conversely, a proactive approach-regular monitoring of gait speed, timely medication adjustments, and scheduled PT/OT sessions-creates a positive feedback loop that reinforces progress.
Insurance providers in many regions, including Australia, have begun to recognize the cost‑effectiveness of early intervention, offering subsidies that mitigate financial barriers.
Nevertheless, systemic obstacles remain, and patients must advocate for themselves, requesting comprehensive assessments without hesitation.
Family members also play a crucial role by observing subtle changes and encouraging prompt medical evaluation.
Technology, such as wearable exoskeletons and AI‑driven gait analysis, is on the horizon and will become most effective when paired with early diagnosis.
Gene‑therapy trials underscore the urgency, as the therapeutic window for editing is narrow and missed opportunities cannot be reclaimed.
In sum, the earlier the diagnosis, the broader the arsenal of treatments available, and the higher the likelihood of preserving autonomy.
Take the first step today, document your symptoms, and schedule that neurological exam-your future self will thank you.